Prevalence < 1/1.106. Rare anomaly of the bronchial divisions. The original description was: a bronchus emerging from the main left trunk, crossing the mediastinum to the middle and lower right lobes (A).
Other variants have been described such as:
.jpg)
where BB = bridging bronchus.
The bridging bronchus originates from a pseudo carina, more (T5 - T7) than the normal carina (T4 - T5). It can exceptionally originate from the right main bronchus (C). In some cases, the bridging bronchus is connected to the whole right lung (E, F). In most cases, the main bronchus is associated to a local or extended stenosis of the airway: the most common localization is the main left bronchus (B) or the trachea. The stenosis is due to a structural anomaly of the trachea (complete tracheal rings without pars membranacea) or to an extrinsic compression by an aberrant retrotracheal left (sling) pulmonary artery (see aortic arch, anomalies. Cases associated with anal imperforation have been described.
In case of aberrant retrotracheal left pulmonary artery, 30 % of the patients present with associated cardiac anomalies (ASD, VSD, Fallot, aortic coarctation) and in 25 % of cases, there is a persistent left superior vena cava (see this term).
In case of aberrant retrotracheal left pulmonary artery, the Wells and Landing classification is used according to the thoracic level of the carina and the anatomy of the bronchial tree:
- type I: carina at the level of the T4 - T5 vertebrae; A: normal tracheobronchial anatomy; B: presence of a tracheal bronchus
- type II: carina at the level of the T5 - T6 vertebrae; A: the bronchial bifurcation has a wide angle; B: absent right mainstream bronchus
.jpg)
Clinical presentation: signs of airway obstruction following intrinsic or extrinsic airway stenosis such as respiratory distress (birth), stridor, wheezing, frequent respiratory infections; ventilation difficulties after intubation, extubation failure. These signs can be masked or complicated by those of an associated cardiac abnormality. Chest X-Ray: sometimes, hyperinflation of the right lung with mediastinal shift to the left.
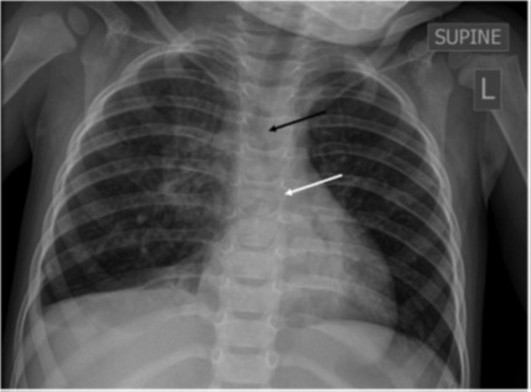
Black arrow: carina; white arrow: pseudo-carina
Diagnosis is difficult: bronchoscopy, thoracic helical CT with reconstruction.
Differential diagnosis with a tracheal bronchus (see this term): the tracheal bronchus connects to the trachea above the normal level of the carina (T4-T5)
The prognosis is poor in case of severe stenosis of the airways.
Treatment: more or less complex tracheoplasty often associated with the correction of the cardiac anomaly or under ECMO.
Anesthetic implications:
preoperative echocardiography; hyperreactivity of the airways; frequent respiratory infections; difficult ventilation or/and intubation (tracheal stenosis, intubation of a tracheal diverticulum); plan to check the position of the distal end of the tracheal tube (fibroscope); controlled pressure ventilation with a high I/E ratio (1/1,5 or 1/1) to counteract the increase in airway resistance and a slow ventilation rate to avoid trapping beyond the stenotic segment. Implications of the associated heart disease.
References :
- Désir A, Ghaye B.
Congenital abnormalities of the intrathoracic airways.
Radiol Clin N Am 2009; 47: 203–25
- Schnabel A, Glutig K, Vogelberg C.
Bridging bronchus: a rare cause of wheezy bronchitis.
BMC Pediatrics 2012; 12: 110
- Shakuo T, Oe K, Shimura Y, Awakura H, Yamada A.
Intraoperative anesthetic management of an infant with a bridging bronchus.
Pediatr Anesth 2018; 28: 815-6.
- Henry BM, Cheruiyot I, Wong L, Keet K, Mutua V, Chhapola V, Tubbs RS.
The bridging bronchus : a comprehensive review of a rare, potentially life-threatening congenital airway anomaly associated with cardiovascular defects.
Pediatr Pulmonol 2019 ; 54 : 1895-1904
- Zikic A, Kritzinger F, Hojo O, Gatt D.
Recurrent bronchiolitis: a bridge to diagnosis.
J Pediatr 2024; 271:114039.
Updated: July 2024