These anomalies constitute less than 1 % of all congenital heart defects but they are susceptible to compress the aerodigestif tract. They are associated with a congenital heart defect in approximately 12 to 32 % of cases, and are frequently found in trisomy 21, Di George syndrome (CATCH 22), CHARGE or PHACE (see those terms).
They have in common to be responsible, during the first two years of life:
- of signs of tracheal compression: stridor (typically inspiratory and expiratory), bronchial congestion, frequent respiratory infections; the presence of total tracheal rings is sometimes associated.
- of signs of esophageal compression: dysphagia for solids.
The diagnosis is made by CT or MRI, and tracheobronchoscopy to evaluate the importance of tracheal compression.
.jpg)
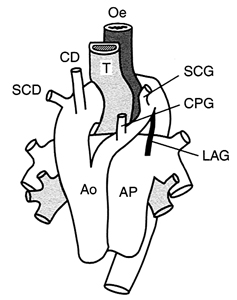
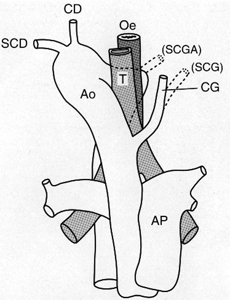
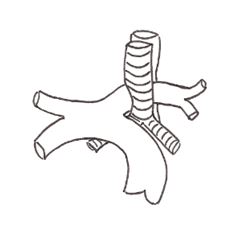
Table: illustration of the main anomalies with in each section: a drawing from the anteroposterior view, from above at the level of Th4 and the opacification of the esophagus (AP and profile view)
There are
1. retro-esophageal subclavian artery (prevalence: 0.6 to 2.3%, more frequent in presence of trisomy 21)
This anomaly is frequent but often asymptomatic when the aortic arch is on the left (retro-esophageal right subclavian artery or Lusoria artery). In case of right aortic arch, the right subclavian artery can be retro-esophageal. The treatment consists in the section of the arterial ligament (fibrous residue of the ductus arteriosus) and/of the artery with reimplantation on the aorta if feasible. An aneurysmal dilatation is o ften observed at the origin of the aberrant subclavian artery: it is known as the Kommerell diverticulum (see this term)
2. Right aortic arch (prevalence: 0.05 - 0.1%)
Several situations:
- right aortic arch with mirror image of the normal anatomical situation; the abdominal aorta finds its normal position to the left at the level of the abdomen
- right aortic arch with an aberrant left subclavian artery (Neuhauser's anomaly): the latter joins the left upper limb by passing in front of the trachea
- right aortic arch with an isolated left subclavian artery (very rare): there is a risk of vascular steal because this artery is fed either by the pulmonary artery via a patent ductus arteriosus or by retrograde flow from the left vertebral artery via the polygon of Willis
3. double aortic arch
it consists of the division of the ascending aorta, which divides into two arches who surround the aerodigestive tract and join after the esophagus. The descending aorta is usually to the right. In case of poor tolerance,the smallest of the two arches has to be removed.
4. cervical aorta
The aortic arch is located higher than normal, above the manubrium. There is a pulsating mass at the base of the neck or in the supraclavicular fossa. Risk of aneurysmal dilatation in adulthood.
The innominate trunk originates on the left of the aortic arch and compresses the trachea anteriorly on its way to the right cervical region. In case of significant respiratory symptoms, one can suspend the innominate trunk and the ascending aorta to the sternal wall (aortopexy).
6. aberrant left pulmonary artery (retrotracheal left pulmonary artery 'pulmonary artery sling')
The left PA arises more on the right than normal (often from the right PA) and travels between the trachea and
esophagus. It is a cause of compression and right tracheobronchomalacia which can cause early respiratory distress with right lobar emphysema or wheezing resistant to treatment or repetitive respiratory infections. If necessary, treatment consists of the reimplantation (with cardiopulmonary by-pass) of this aberrant PA in front of the trachea. Chronic compression can lead to tracheomalacia.
Several types are known (Wells and Landing classification according to the position of the artery in relation to the carina):
- type 1: the carina is at the level of T4 - T5 and tracheobronchial anatomy is normal
- type 2: the carina is at the level of T5 -T6; the angle of the bronchial bifurcation is widened and bronchial anatomy can be modified

A cardiac anomaly is associated in 30 % of cases: ASD, VSD, Fallot tetralogy, DORV (double-outlet right ventricle). A left upper vena cava (see this term) is present in 25 % of cases. Pulmonary anomalies are not rare, with pulmonary hypoplasia or even agenesis
Anesthetic implications:
echocardiography: associated malformation ?airway obstruction, hyperreactivity of the airway. Risk of post-operative tracheomalacia. Care should be taken in case of esophagoscopy or prolonged use of a gastric tube: a few cases of hematemesis due to fistulisation of the compressed esophagus into the mispositioned vessel have been reported.
References :
- Kussman BD, Geva T, McGowan FX.
Cardiovascular causes of airway compression.
Pediatr Anesth 2004; 14:60-74.
- Turner A, Gavel G, Coutts J.
Vascular rings: presentation, investigation and outcome.
Eur J Pediatr 2005; 164: 266-70.
- Van Woerkum F, Bont L, Haas F, Freund M, van Gestel S.
Aortoesophageal fistula due to double aortic arch and prolonged nasogastric intubation: case report and review of the literature.
Eur J Pediatr 2006; 165: 660-1.
- Cannavale A, Francone M, Galea N, Roggini M, Carbone I.
Three-dimensional Magnetic resonance imaging of Kommerell diverticulum in a child with recurrent dysphagia.
J Pediatr Surg 2010; 45: 2092-3.
- Fuentes S, Cano I, Lopez M, Moreo C et al.
Arterial-oesophageal fistula: a severe complication in children with cardiovascular abnormalities.
Pediatr Surg Int 2010; 26: 335-7.
Updated: May 2023