Prevalence 1/450, ie 0.1 to 0.3 % of the population. Cardiac rhythm disorder caused by electrical ventricular pre-excitation following the absence of regression of some fetal conductive fibers: therefore, there may be several types of connections between the right atrium and ventricles. The most common is an aberrant connection (Kent bundle) between the bundle of His and the myocardium. In case of connection between the atrium and the bundle of His, there is a short PR without δ wave called Lown-Ganong-Levine syndrome (see this term).
Some patients remain asymptomatic throughout life; however, this anomaly can cause bouts of supraventricular tachycardia (Bouveret disease), but also of atrial fibrillation (20 %) (dangerous because of the wide QRS), atrial flutter (7 %) or ventricular fibrillation. In 40 % of cases it is associated with a congenital heart disease: Ebstein anomaly or transposition of the great vessels. It can also be present in case of hypertrophic cardiomyopathy, Pompe disease or Danon disease. There are about 5 % of familial cases associated with a mutation of the PRKAG2 gene (7q36.1) [MIM 216 740] (cardiomyopathy due to glycogenosis) or BMP2 gene (microdeletion 20p12.3).
_EN.jpg)
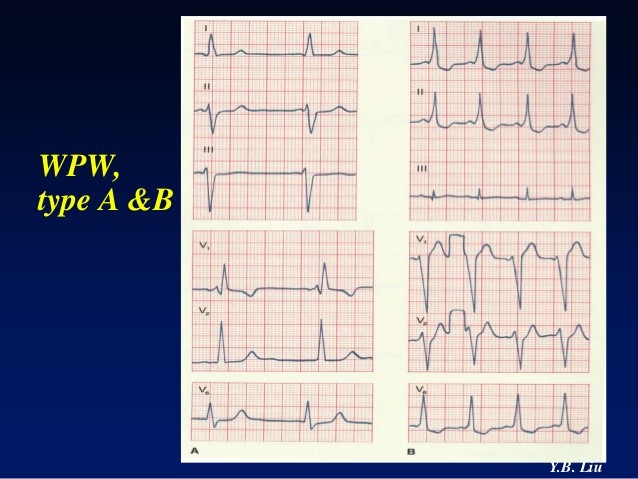
Three possible presentations of WPW: A: sinusal tachycardia 152/min with short PR and delta wave B: supraventricula tachycardia with narrow QRS complexes (215/min) without identifiable P wave C: atrial fibrillation with wide complexes (300/min) (from G. Vaksmann)
The ECG at rest typically shows a short PR (< 120 msec) and a widened QRS with a δ wave.
There are two forms:
- type A: caused by a left aberrant pathway : short PR, δ wave and tall R wave with inverted T waves in V1-V3 : picture of pseudo right ventricular hypertrophy, negative δ wave in avL
- type B: caused by a right accessory pathway : short PR, negative δ wave and S wave in V1 (pseudoinfarct), tall R waves and inverted T wave in V4-6 : picture of left ventricular hypertrophy
However, in case of abnormal retrograde conduction (from ventricle to atrium), the ECG is normal when the rhythm is sinusal and the diagnosis can only be made during an episode of supraventricular paroxysmal tachycardia. There are also intermittent forms of WPW (13 % in children) in which the tracing normalizes with stress: the risk of supraventricular tachycardia is the same as in the permanent forms.
During supraventricular tachycardia crisis, the reentry phenomenon generally occurs in a retrograde way through the accessory pathway: it is referred as orthodromic tachycardia with fine QRS (or sometimes with an image of bundle branch block). More rarely, the normal conduction is via the accessory pathway and reentry via the normal pathway: it is referred as antidromic tachycardia with wide QRS.
The main risk is a crisis of paroxysmal supraventricular tachycardia; the crisis can be dealt with by vagal maneuvers (carotid sinus massage, Valsalva maneuver, compression of eyeballs) if it is well-tolerated; otherwise: rapid IV injection of adenosine or cardioversion (0.5 to 1J/kg for the first shock) are needed. Digitalis is contraindicated because it shortens the refractory period of the accessory bundle of Kent and therefore worsens tachycardia. Treatment is based on cordarone or a β-blocking agent. If the refractory period of the accessory bundle is less than 220 ms, its destruction by radiofrequency should be considered.
Anesthetic implications:
monitor ECG: tachyarrhythmias. In case of atrial fibrillation, verapamil and digoxin are contraindicated. Avoid inducing tachycardia and prevent sympathetic stimulation, which may trigger supraventricular tachycardia.
Schedule administration of adenosine to avoid a long sinusal pause post-injection
(Dr. Guy Vaksmann, Lille)
|
Preparation: < 10 kg: 1 ampoule of adenosine ad 20 ml with 0.9% NaCl 10-20 kg: 2 ampoules of adenosine ad 20 ml with 0.9% NaCl < 20 kg: 4 ampoules of adenosine ad 20 ml with 0.9% NaCl Administration: 3 ways stopcock + short IV extension line + 1 syringe 0.9% NaCl - inject 1 ml rapidly + flush - wait for 1 minute; if failure: inject 2 ml and wait for 1 minute Dose max: 1 ml/kg or 5 ml if > 10 kg
|
References :
- van der Starre PJA.
Wolff-Parkinson-White syndrome during anesthesia.
Anesthesiology 1978 ; 48 : 369-72.
- Richmond MN, Conroy PT.
Anesthetic management of a neonate born prematurely with Wolff-Parkinson-White syndrome.
Anesth Analg 1988; 67: 477-8.
- Abraham EL, Jahr JS, Gitlin MC.
Anesthetic management of a child with Wolff-Parkinson-White syndrome and bronchial asthma.
Am J Anesthesiol 1997; 24:151-3.
- Villain E.
Tachycardies jonctionnelles réciproques et voies accessoires.
in Les troubles du rythme cardiaque chez l’enfant, éditeurs : J Kachaner, E Villain, Médecine-Sciences Flammarion, 2006, p55-64
- Vaksmann G, Bouzguenda I, Richard A.
Troubles congénitaux du rythme cardiaque chez l’enfant: quelles recommandations pour l’anesthésie?
Anesth Réanim 2016 ; 2: 316-20
- Larson N P, Rosenthal J B, Bridwell R E, et al.
Hide and seek: intermittent preexcitation Wolff-Parkinson-White : case report and management overview.
Cureus 2020 ; 12: e8971.
Update: March 2021