(Feto-Fetal Transfusion Syndrome, FFTS)
Prevalence: 1-3/10,000 births. This complication occurs in 8 to 10 % of biamniotic monochorial twin pregnancies, where both fetuses share the same placenta but are present in two distinct amniotic pouches. The twins' umbilical cords fit on the same placenta and are connected by blood vessels. There are arterioarterial and venovenous anastomoses on the surface of the placenta, and arteriovenous anastomoses deeper inside. There could be a smaller amount of arterioarterial anastomoses and an increase in arteriovenous anastomoses in case of STT: this leads to an imbalance of circulation and blood is transferred disproportionately from one of the twins (the donor) to the other (the recipient):
- the recipient twin has a volume overload mechanically compensated by the increase in urine production, which creates an excess of amniotic fluid (hydramnios). It will often be larger than its twin (by anasarca) and may suffer from heart failure;
- the donor twin may have a decrease in blood pressure, hypotrophy (small fetus), a small bladder and sometimes anemia. It does not produce urine and therefore no amniotic fluid (oligoamnios).
Quite paradoxically this phenomenon does not occur, despite the presence of the same anastomoses, in monochorial-monoamniotic pregnancies.
If it develops in early pregnancy (before 26 weeks), this syndrome can cause fetal death or severe disabilities.
Main sign: combination of a polyuric hydramnios in the recipient twin and an oliguric oligoamnios in the donor twin.
Quintero's classification is used to assess the severity of the syndrome in utero:
- stage I: oligamnios and hydramnios, the bladder of the donor twin is visible
- stage II: oligamnios and hydramnios, the bladder of the donor twin is invisible
- stage III: oligamnios and hydramnios + abnormality of at least one echo Doppler: the diastolic flow in the umbilical artery of the donor is null or reversed, or the diastolic flow in the ductus venosus of the recipient is null or reversed, or the umbilical vein is pulsatile
- stage IV: pleural or pericardial effusion or ascites or anasarca in the receiving twin
- stage V: death of one fetus
Treatments:
- repeated amniocentesis is the oldest technique. However, it treats the symptom and not the pathology. It consists of removing 1 to 2 liters of amniotic fluid from the recipient's pouch, using a needle. Drainages are repeated if the hydramnios reappears. Because serial amniocentesis increases the risk of preterm birth, it is not performed in early pregnancy.
- laser coagulation of the anastomoses. under percutaneous local anesthesia. A 2 mm diameter endoscope bearing a diode laser fiber is introduced under local anesthesia into the amniotic cavity through a 3 mm diameter needle. With the help of echography, fetoscope and laser, anastomoses between the two twins are coagulated. The coagulation of the chorionic plaque anastomoses allows the survival of at least one twin in about 80 % of cases with an average term at birth of 33 weeks and a risk of sequelae in survivors of less than 10 %, mainly related to prematurity.
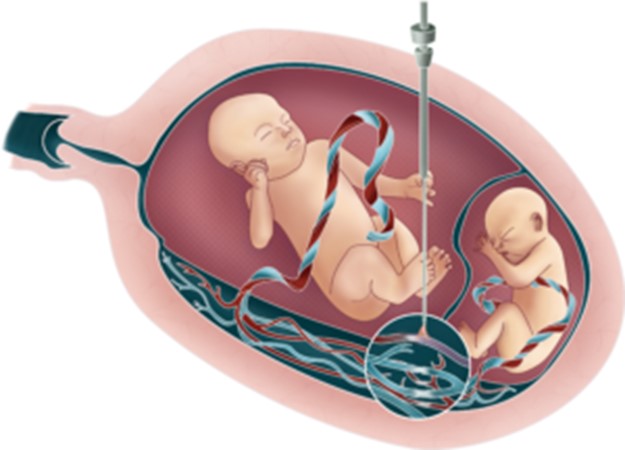
- coagulation of the umbilical cord of one of the twins. An interruption of the most affected twin may be requested by parents in order to preserve the life of the other. The procedure involves coagulating the umbilical cord of the affected fetus, resulting in death. This fetus is left in the mother's womb while the other fetus continues to develop until birth.
Anesthetic implications:
birth is often premature.
In the donor twin: intrauterine growth retardation, anemia ? kidney function ?
In the recipient twin: echocardiography (hypertrophic cardiomyopathy ? pulmonary artery stenosis ?), polycythemia ?
References :
-
Updated: November 2021