[MIM 604 772, 611 938, 614 021, 614 916, 615 441].
The prevalence is estimated at 1-5/10,000. It is a cardiac arhythmogenic disease due to calcium channelopathy.
Different forms have been identified:
1) juvenile forms :
- CPVT1 [MIM 604 772]: dominant autosomal form (mutation of the RYR2 gene (ryanodine cardiac receptor) (1q43) involved in 55 to 65 % of cases; median age at onset: 10 years
- CPVT2 [MIM 611 938]: autosomal recessive form; mutation of the CASQ2 gene coding for calsequestrin (1p13.1), involved in about 1 % of cases; median age at onset: 7 years
- CPVT3 [MIM 614 021]: autosomal recessive form; mutation of the TECRL gene (4q13.1); median age at onset: 10 years
- CPVT4 [MIM 614 916]: autosomal recessive form; mutation of the CALM1 gene (14q32.11) coding for calmodulin; median age at onset: 4 years
- CPVT5 [MIM 615 441]: autosomal recessive form; mutation of the TRDN gene (6q22) coding for triadin; median age at onset: 2 years
- CPVT6 [MIM 618 782]: autosomal recessive form; mutation of the CALM3 gene (19q13).
Some cases of mutations of the KCNJ2 gene (17q23), also associated with Andersen-Tawil syndrome (see this term), and of the SNTA1 gene (20q), other mutations of which cause long congenital QT type 12, have been described.
2) the adult form (30 % of cases) affects women more than men.
Clinical presentation: syncopes triggered by stress or emotion. Sudden death is inaugural in 10 to 20 % of cases: 31 % mortality before 30 years of age.
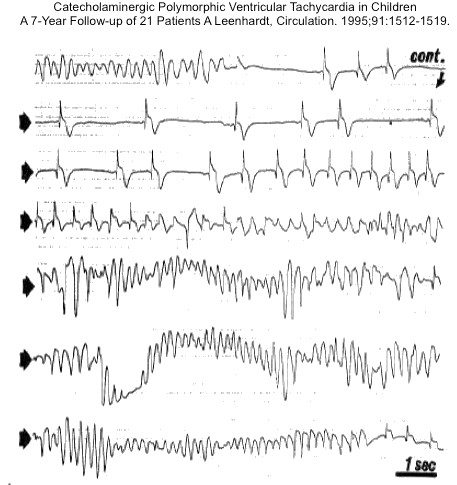
The ECG is normal at rest; during a crisis: polymorphic or bidirectional TV when two different morphologies of QRS are present (stress test or test with isoprenaline or on Holter); typically, extrasystoles appear when the heart rate reaches 110-130 bpm: sometimes: association of supraventricular tachycardia and atrial fibrillation.
Treatment: β-blocking agents (nadolol, propranolol) in high doses, or flecainide; in case of failure, implantable defibrillator or even denervation of the left ventricle.
Anesthetic implications:
there is no risk of malignant hyperthermia despite the mutation of the cardiac isoform of the ryanodine receptor gene; keep esmolol ready and place the defibrillation pads on the patient's chest; avoid stress (premedication, parental presence), ketamine and any factor susceptible to increase the circulating catecholamines level; avoid an heart rate exceeding 120/min as it is often a triggering threshold.
Dexmedetomidine is a good choice because of its alpha-2-adrenergic and sedative properties. In case of cardiac arrest, adrenaline exacerbates the rhythm disorders and amiodarone is useless.
In case of regional anesthesia: avoiding the addition of adrenaline to the local anesthetic solution ? A high thoracic epidural block can be used to test the efficacy of a cardiac denervation.
References :
- Sawn H, Laitinen PJ, Toivonen L.
Volatile anesthetics and succinylcholine in cardiac ryanodine receptor defects.
Anesth Analg 2004 ; 99 : 435 - Garabedian L, Verryckt A, Panzer J, De Wolf D.
Catecholaminergic polymorphic ventricular tachycardia in a child: a case report.
Acta Paediatrica 2008; 97: 127-9. - Chen SY, Cucchiaro G, Bushman G.
The role of thoracic epidural blockade in predicting responsiveness to left sympathetic denervation in patients with catecholaminergic polymorphic ventricular tachycardia.
J Cardiothorac Vasc Anesth. 2011;25:844-6. - Cafferkey A, McMahon C.
Successful treatment of refractory cardiac arrest with blockade and extracorporeal life support in a pediatric patient with catecholaminergic polymorphic ventricular tachycardia : a case report.
A&A Practice 2018; 11(3): 63-67 - Omiya K, Mitsui K, Matsukawa T.
Anesthetic management of a child with catecholaminergic polymorphic ventricular tachycardia undergoing insertion of implantable cardioverter defibrillator : a case report.
JA Clinical Reports 2020; 6 :16
Updated: September 2022