(Charcot disease, Lou Gehrig's disease)
Rare: 1/20,000 in Western Europe, more prevalent in the Western Pacific Islands.
Neurodegenerative disorder due to the degeneration of motorneurons in the motor cortex, the corticospinal pathway, brain stem and spinal cord. Most cases are sporadic but 5-10 % are familial.
Identified types and forms:
- the classic, sporadic form: several favoring factors have been identified such as smoking, repeated cerebral microtraumatisms (contact sport, boxing).
- familial forms:
- type 1 : autosomal dominant or recessive transmission of a mutation of the SOD1 gene (21q22.11) coding for the superoxide dismutase Cu/Zn [MIM 105 400]
- type 2 or juvenile : autosomal recessive transmission of a mutation of the ALS2 gene (2q33.1) coding for alsin [MIM 105 100]
- type 3 : autosomal dominant transmission of a mutation of a gene (18q21) [MIM 606 640]
- type 4 or juvenile: autosomal dominant transmission of a mutation of the SEXT1 gene (9q34.14) coding for senataxin [MIM 602 433]
- type 5 or juvenile : autosomal recessive transmission of a mutation of the SPG11 gene (15q21.1) coding for spatacsin [MIM 602 099]
- type 6, with or without frontotemporal dementia : autosomal dominant transmission of a mutation of the FUS gene (16p11.2) [MIM 608 030]
- type 7 : autosomal dominant transmission of a mutation of a gene in 20p13 [MIM 608 031]
- type 8 : autosomal dominant transmission of a mutation of the VAPB gene (20q13.32) coding for a protein associated with the vesicular membrane [MIM 608 627]
- type 9 : autosomal dominant transmission of a mutation of the ANG gene (14q11.2) coding for angiogenin [MIM 611 895]
- type 10, with or without frontotemporal dementia: autosomal dominant transmission of a mutation of the TARDBP gene (1p36.22) [MIM 612 069]
- type 11 : autosomal dominant transmission of a mutation of the FIG4 gene (6q21) [MIM 612 577]
- type 12 : autosomal dominant or recessive transmission of a mutation of the OPTN gene (10p13) coding for optineurin [MIM 613 435]
- type 13 : autosomal dominant transmission of a mutation of the ATXN2 gene (12q24.12) coding for ataxin 2 [MIM 183 090]
- type 14, with or without frontotemporal dementia : autosomal dominant transmission of a mutation of the VCP gene (9p13.3) coding for a protein associated valosin [MIM 613 954]
- type 15, with or without frontotemporal dementia : X-linked transmission of a mutation of the UBQLN2 gene (Xp11.21) coding for ubiquilin 2 [MIM 300 857]
- type 16 or juvenile : autosomal recessive transmission of a mutation of the SIGMAR1 gene (9p13.3) [MIM 614 373]
- type 17 : autosomal dominant transmission of a mutation of the CHMP2B gene (3p11.2) [MIM 614 696]
- type 18 : autosomal dominant transmission of a mutation of the PFN1 gene (17p13.2) coding for profilin 1 [MIM 614 808]
- type 19 : autosomal dominant transmission of a mutation of the ERBB4 gene (2q34) [MIM 615 515]
- type 20 : autosomal dominant transmission of a mutation of the HNRNPA1 gene (12q13.13) coding for a nuclear ribonuclear protein [MIM 615 426]
- type 21 : autosomal dominant transmission of a mutation of the MATR3 gene (5q31.2) coding for matrin 3 [MIM 606 070]
- type 22, with or without frontotemporal dementia : autosomal dominant transmission of a mutation of the TUBA4A gene (2q35) coding for tubulin alpha 4A [MIM 606 070]
- type 23 : autosomal dominant transmission of a mutation of the ANXA11 gene (10q22.3) coding for annexin A11 [MIM 617 938]
- type 24 : susceptibility to lateral amyotrophic sclerosis due to a mutation of the NEK1 gene (4q33) [MIM 617 892]
- type 25 : susceptibility to lateral amyotrophic sclerosis due to the autosomal dominant transmission of a mutation of the KIF5A gene (12q13.3) [MIM 617 921]
- form associated to the NEFH gene : autosomal dominant or recessive transmission of a mutation of the NEFH gene (22q12.2) coding for a neurofilament [MIM 105 400]
- form associated to the PRPH gene : autosomal dominant transmission of a mutation of the PRPH gene (12q13.12) coding for peripherin [MIM 105 400]
- form associated to dynactin 1 : autosomal dominant transmission of a mutation of the DCTN1 gene (2p13.1) coding for dynactin 1 [MIM 105 400]
- amyotrophic lateral sclerosis and/or frontotemporal dementia : autosomal dominant transmission of a mutation of the C9orf72 gene (9p21.2) [MIM 105 550]
- amyotrophic lateral sclerosis and/or frontotemporal dementia : autosomal dominant transmission of a mutation of the CHCHD10 gene (22q11.23) [MIM 615 911]
- amyotrophic lateral sclerosis and/or frontotemporal dementia : autosomal dominant transmission of a mutation of the SQSTM1 gene (5q35.3) [MIM 616 437]
- amyotrophic lateral sclerosis and/or frontotemporal dementia : autosomal dominant transmission of a mutation of the TBK1 gene (12q14.2) [MIM 616 439].
- the so-called 'Western Pacific' form: in the island of Guam, it seems related to the accumulation of beta-methylamino-L-alanine in the brain tissue. This molecule is a neurotoxin produced by a blue-green alga that resides on the roots and in the seeds of the sago palm (cycad).
Uncertain pathophysiology: progressive destruction of motoneurons following decreased elimination of glutamate by astrocytes; aggregation of proteins in the cytoplasm or axons; loss of the GABAergic inhibitory control of the cortical motoneurons, etc...
The symptomatology is highly variable and depends on the topography of the affected motorneurons ; the impairment may be initially unilateral or localized:
* spinal motoneurons (2/3 of cases): muscle weakness and atrophy; spasticity; twitching; hyperreflexia; clonus
* bulbar motoneurons: dysarthria, dysphagia, laryngeal spasms, sialorrhea
* in case of bilateral involvement of the cortico-bulbar tracts: emotional crises: paradoxical tears and laughter
* the involvement of the respiratory muscles leads to paradoxical breathing, tachypnea with air hunger; obstructive sleep apnea
* there is no sensory disturbances nor loss of control of the sphincters; cognitive functions remain intact
Diagnosis: EMG
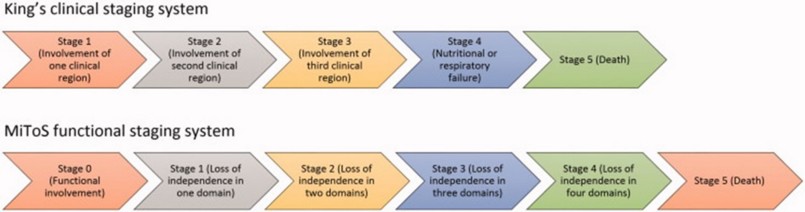
Disease progression is assessed using the King's College classification or the MiToS scale:
Prognosis: bad: progressive respiratory insufficiency with death within 3-5 years.
Treatment:
- symptomatic: physiotherapy, non invasive ventilation, gastrostomy...
- antispastics: baclofen, dantrolene, tizanidine, botulinum toxins
- riluzole: it reduces the concentration of glutamate at the level of nerve endings, by blocking postsynaptic NMDA receptors; sometimes increase in liver enzymes, high BP
- high dose vitamin B12
- ceftriaxone, a beta-lactam antibiotic that increases one of the glutamate transporters
- dexpramipexole: an antioxidant used as antiparkinsonian agent
- pacing of the diaphragm ?
Anesthetic implications:
evaluate respiratory function: SpO2 when breathing room air, functional tests, cough; risk of pulmonary aspiration: extubation when completely awake; avoid succinylcholine: cases of hyperkalemia have been described. If NIV is used, it should be continued immediately post-operatively; in the event of major respiratory insufficiency, O2 supplementation should be used with caution. Curarization with caution: one case of incomplete antagonization of rocuronium by sugammadex has been described.
Several cases of lumbar epidural anaesthesia or spinal anaesthesia combined with sedation (propofol, dexmedetomidine or remimazolam) have been described without worsening the clinical course.
References :
- Kwon Y-S, Lim Y-H, Woo S-H, Yon JH, Kim K-M. Epidural anesthetic management of a patient with amyotrophic lateral sclerosis (ALS). Korean J Anesthesiol 2009; 57: 361-3
- Prabhakar A, Owen CP, Kaye AD.
Anesthetic management of the patient with amyotrophic lateral sclerosis.
J Anesth 2013; 27: 909-18.
- Sertöz N, Karaman S.
Peripheral nerve block in a patient with amyotrophic lateral sclerosis.
J Anesth 2012; 26: 314-5.
- Turner M, Lawrence H, Arnold I, Ansorge O, Talbot K.
Catastrophic hyperkalaemia following administration of suxamathonium chloride to a patient with undiagnosed amyotrophic lateral sclerosis.
Clin Med 2011; 11: 292-3
- Thourot M, Cornillon B, Robert R, Royer D, Patrigeon R-G.
Hyperkaliémie menaçante suite à une injection de succinylcholine orientant le diagnostic vers une sclérose latérale amyotrophique.
Anesth Réanim 2017 ; 3 : 193-7.
- Fang T, Al Khleifat A, Stahl DR, Lazo la Torre C, Murphy C et al.
Comparison of the King’s and MiToS staging systems for ALS.
Amyotrophic Lateral Sclerosis and Frontotemporal Degeneration 2017; 18: 227-32
- Benarroch L, Bonne G, Rivier F, Hamroun D.
The 2020 version of the gene table of neuromuscular disorders.
Neuromusc Dis 2019 ; 29 : 980-1018 or http://www.musclegenetable.fr
- Hoeper AM, Barbara DW, Watson JC, Sprung J, Weingarten T.
Amyotrophic lateral sclerosis and anesthesia: a case series and review of the literature.
J Anesth 2019; 33: 257-65.
- Panchamia JK, Gurrieri C, Amundson AW.
Spinal anesthesia for amyotrophic lateral sclerosis patient undergoing lower extremity orthopedic surgery: an overview of the anesthetic considerations.
International Medical Case Reports Journal 2020 ; 13 : 249-54
- Chun HR, Chung J, Kim NS, Kim AJ, Kim S, Kang KS.
Incomplete recovery from rocuronium-induced muscle relaxation in patients with amyotrophic lateral sclerosis using sugammadex: A case report.
Medicine 2020;99:3 (e18867).
- Nimma S, Gans A, MD,Wardhan R, Allen W.
Remimazolam sedation and neuraxial anesthesia in a patient with amyotrophic lateral sclerosis undergoing an open colectomy: a case report.
A&A Practice 2023;17:e01733
Updated: January 2024