(scimitar anomaly, Halasz syndrome, congenital venopulmonary syndrome, Felson venolobar syndrome)
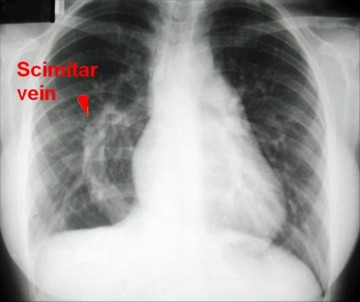
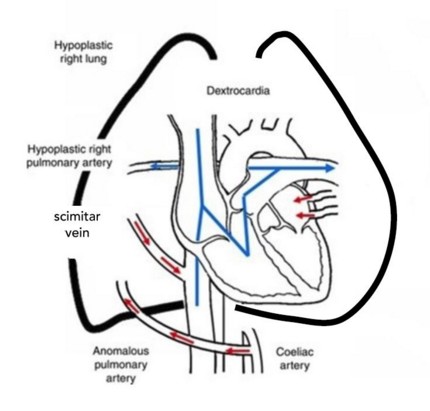
Prevalence: between 1 to 3/100,000. Female predominance. Mutation on locus 4q12 in many patients. It is an abnormal form of partial pulmonary venous return where part (generally the lower lobe) or all (30 % of cases) of the pulmonary venous return from the right lung is drained into the inferior vena cava or right atrium. The name of scimitar syndrome comes from the convex shadow in the right lung field), similar to a Turkish sword, on imaging (AP X-Ray or angiography).
Associated clinical anomalies:
- a variable hypoplasia of the right pulmonary arterial vascularization and of right lung (often bilobar)
- a cardiac dextroposition related to the right pulmonary hypoplasia
In addition, the following elements can be present too :
- systemic vascularization of part of the right lung (differential diagnosis of the lobar sequestrations) (see this term).
- a cardiac malformation (25 %): ASD (80 %), aortic arch hypoplasia or aortic coarctation, patent ductus arteriosus (75 %), tetralogy of Fallot, VSD (30 %), pulmonary vein stenosis (20 %), aortopulmonary collaterals
More rarely: right diaphragmatic hernia, bronchogenic cyst, horseshoe lung or agenesis of the pericardium.
The clinical presentation is variable:
- heart failure with pulmonary hypertension in the neonatal period,
- frequent respiratory infections (bronchodilators are poorly effective)
- fortuitous finding depending on the importance of the left-right shunt.
For example,
- in the absence of systemic vascularization of the right lung: intrapulmonary shunt via the pulmonary artery with the dilatation of the RA thenprogressive right ventricular hypertrophy
- in case of hypoplasia of the pulmonary artery and systemic vascularization: pulmonary arterial hypertension and left-to-right shunt; sometimes, systemic arterio-venous fistula with risk of cardiac decompensation.
The forms that are symptomatic before the age of one year are often referred to as "infantile or juvenile" and have a very poor prognosis because of the associated abnormalities.
Diagnosis:
- chest X-Ray: dextroposition of the heart, hypoplasia of the right lung, picture of the right paracardiac scimitar
- echocardiography: visualization of the scimitar vein (monophasic flow without inversion during atrial contraction) and its connection with IVC.
- 3D CT and cardiac catheterization.
Treatment: surgery (right lobectomy, reimplantation of the abnormal vein in the L.A.) or interventional catheterization (embolization of the systemic vasculature of the right lung), depending on the associated abnormalities.
Anesthetic implications:
according to the clinical presentation: heart failure; left to right 'fixed' shunt, obstructive syndrome poorly responsive to bronchodilators (lung hypoplasia). Echocardiography and SpO2 at room air. Risk of desaturation and hypotension when the patient is lying on his left side.
References :
- Chemin A, Bonnet D, Le Bourgeois M, Levy M, Delacourt C.
Respiratory outcome in children with Scimitar syndrome.
J Pediatr 2013; 275-9.
- Wang CC, Wu ET, Chen SJ, Lu F, Huang SC, Wang JK et al.
Scimitar syndrome : incidence, treatment and prognosis.
Eur J Pediatr 2008; 167: 155-60.
- Singh A, Sharma N.
Anaesthetic Management of Scimitar Syndrome: A Case Report.
The Indian Anaesthetists’ Forum – (http://www.theiaforum.org) Online ISSN 0973-0311, July 2010
- Alberti N, Espérable F, Stéphant E, Lamblin A et al.
Découverte fortuite d’un syndrome du cimeterre au cours d’une visite systématique: à propos d’un cas.
Médecine et Armées 2011 ; 40 : 111-4.
- Hasan M, Varshney A, Agarwal P.
A case of scimitar syndrome: anaesthetic considerations regarding non-cardiac surgery.
Ped Anesth Crit Care J 2016; 4: 89-91
- Sergin D, Tanatti B, Ulukaya S.
Positional oxygenation changes in an adult patient with Scimitar syndrome: a case report.
A&A Practice 2018; 11: 247-9
Updated: August 2021