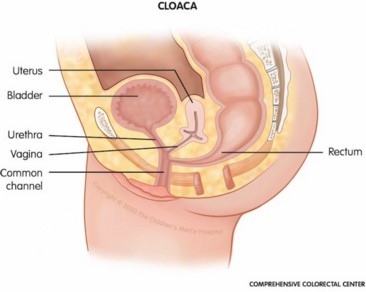
Incidence: 1/50,000 births. Persistence of a cloaca is the most complex and rare form of anorectal malformation (see this term). It occurs only in girls. There is only one perineal orifice. The digestive and urogenital tracts end up into a common channel. Other malformations of the vagina (hydrocolpos in 30 % of cases, duplication, septum ...), uterus (bifidity) and urinary tract (ureteral ectopia, reflux ...) are often associated.
The same malformative (VACTERL, etc) or non-malformative associations can be present as in the other anorectal malformations (see this term)
The forms with a short common channel (< 3 cm) are often differentiated from those with a long common channel (> 3 cm).
A distinction is made between:
- forms with a very short common channel (< 1cm) or type1
- forms with short common channel (< 3 cm) and urethra > 1.5cm long
- forms with long common canal (> 3 cm) and urethra < 1.5 cm long
This distinction is important for choosing the best surgical approach and establishing a functional prognosis.
Another distinction is made between
- cloacal dysgenesis: where the common canal is not open to the skin: ascites, anamnios, hydrocolpos, very poor prognosis
- posterior cloaca: this is a persistence of the cloaca where the single orifice is posterior and a functional anal sphincter is present.
Development in the neonatal period requires careful endoscopy of the cloaca, ultrasound (vagina and urinary tract: hydrocolpos ? dilation of the urinary tract ?). Endoscopy and 3D reconstruction of the pelvis are required before subsequent procedures.

This malformation requires a multidisciplinary approach and multiple interventions.
Surgical management is done in at least three stages:
- neonatal period: colostomy often associated with drainage of the hydrocolpos;
- surgical correction between 6 and 12 months:
- very short form: no intervention on the urethra; plasty of the orifice and posterior sagittal anorectoplasty (PSARP)
- common canal < 3 cm and urethra > 1.5 cm: total urogenital mobilization and PSARP sometimes associated with a laparotomy or laparoscopy if the rectum is located highly in the pelvis
- common canal > 3 cm and urethra < 1.5 cm: urogenital separation that allows the use of the common canal as an urethra and PSARP. Vaginoplasty (with ileum, colon or rectum) is performed later
- closure of the colostomy.
Regular monitoring of anal caliber, renal function and gynecological anatomy.
Anesthetic implications:
cardiac, renal and lumbosacral spine and cord echography; neonatal anesthesia. Frequent anesthesia. In the absence of abnormalities of the lumbosacral canal or cord, caudal or lumbar epidural block may be combined with general anesthesia for each of these procedures. In case of combined approach, the maneuver consisting in turning the child 'en bloc' must be synchronized with the surgical team to maximize safety and limit the risk of extubation and/or pulling out catheters in a child covered with surgical drapes.
References :
- Levitt, MA, Peña A.
Cloacal malformations: Lessons learned from 490 cases.
Semin. Pediatr. Surg. 2010, 19, 128–138.
- Wood RJ, Reck-Burneo CA, Levitt MA.
Cloacal malformations: technical aspects of the reconstruction and factors which predict surgical complexity.
Frontiers in Pediatrics 2019 ; doi 10.3389/fped2019.0024
- Jacobs SE, Tiusaba L, Al-Shamaileh T, Bokova E, Russell TR, Ho CP, Varda BK et al
Fetal and Newborn Management of Cloacal Malformations
Children 2022, 9, 888. doi.org/10.3390/children9060888
Updated: September 2022