Estimated incidence: 1/106. Most frequency between 50 and 60 years of age: very rare in children. Some cases have been described after 9 years of age for the deep form, and between 5-8 years of age for the superficial form; some cases are of paraneoplastic origin.
Group of bullous autoimmune dermatological diseases. IgG autoantibodies are directed against desmogleins 1 and or 3 (Ca-dependent proteins of the family of the cadherins located on the surface of keratinocytes at the level of the desmosomes), at the intercellular junctions of the cells of the epidermis and/or the mucous membranes. All areas covered by a malpighian epithelium can therefore be affected. This leads to the destruction of the intercellular junctions (acantholysis), and to the isolation of the cells, causing flaccid blisters on the skin (blister = liquid collection > 10 mm in diameter) and mucosal erosions. Blisters cause painful and extensive erosions, first on the oral and next other mucous membranes and then on the skin.
About half of patients have only oral erosions, that break down and become chronic and painful lesions. Dysphagia and poor food intake are common because the upper part of the esophagus can be involved with dysphagia. Skin bubbles appear on seemingly normal skin and, when ruptured, leave erosion and eventually a crust. The absence of pruritus is usual. Erosions often become infected.
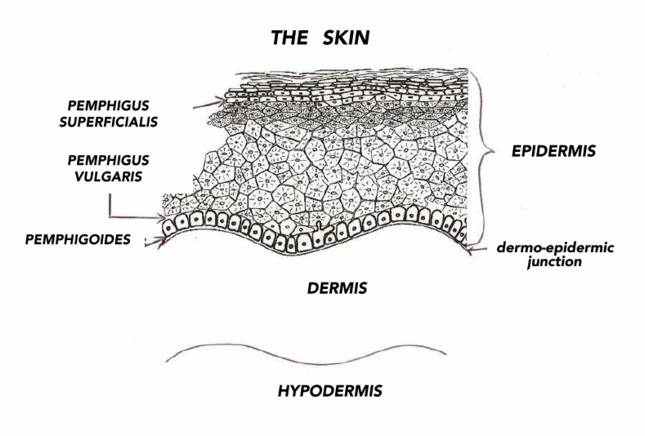
Different forms of pemphigus are listed, according to the involved desmoglein:
• pemphigus vulgaris or deep (75 %) where desmoglein 3 and sometimes 1 are destroyed. It can involve the mucosae and the skin according to the type.
- mucous pemphigus vulgaris. Any mucosa can be involved: eyes, genitalia, mouth, nose, esophagus and anus. The skin is rarely involved.
- mucocutaneous pemphigus vulgaris. The skin and the mucosae are involved. Blisters appear first on oral mucosa, thereafter on the other mucosae and finally on the skin.
Two clinical signs are specific for pemphigus vulgaris:
♦ Nikolsky's sign: the superficial epidermal layers close to blisters slide laterally under the slightest pressure or friction on the skin
♦ Asboe-Hansen's sign: a slight pressure on an intact blister causes the diffusion of the fluid outside the zone of pressure and around the blister.
• pemphigus superficialis (or erythematous, or foliaceous) where desmoglein 1 is destroyed. It only involves the skin of the face, scalp, chest, arms and legs.
• paraneoplastic pemphigus , where desmoglein 1 and 3 are destroyed as well as plakines (other proteins of desmosomes). The skin and the mucosae of the mouth and the esophagus are involved, and it can also involve the lungs. The primary responsible tumor can be benign or malignant, the most common being a non-Hodgkinian lymphoma
• benign familial pemphigus or Hailey-Hailey syndrome (see this term)
• pemphigoides: the intercellular junctions are destroyed at the level of the dermo-epidermic junction
• neonatal pemphigus: the mother with a pemphigus can transfer her autoantibodies to the fetus. The neonate is born with lesions. These lesions disappear after 8 to 10 months of time, following the progressive elimination of the maternal autoantibodies.
Treatments:
Local treatments are similar to those for medium-severity burns (e.g., hydrocolloid dressings).
Systemic treatment aims at reducing the production of the pathogenic autoantibodies: systemic corticosteroid therapy, immunosuppressants such as rituximab, methotrexate, cyclophosphamide, azathioprine, mycophenolate mofetil or cyclosporin. Plasma exchanges and high-dose IV gammaglobulins to decrease Ac levels are also quite effective. Some teams prefer a treatment combining minocycline and nicotinamide combined with local corticosteroid therapy. Minocycline can be replaced by doxycycline.
Contact: pemphigus.asso.fr
Anesthetic implications:
drug interactions with the systemic treatment. Fragile skin and mucous membranes: careful securing of the dressings and intrabuccal maneuvers (detachments, bleeding), skin protection (pressure points).
References :
-
Updated: April 2020