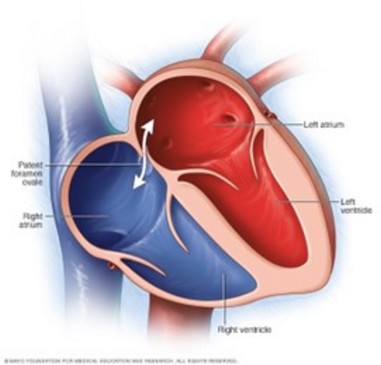
(PFO, acronym for Patent Foramen Ovale)
Common cardiac abnormality: it was found in more than 25 % of cases in an autopsy series. This prevalence is identical in both sexes.
The foramen ovale (Botal hole) is a "baffle"-like passage between the two main constituents of the interatrial septum, the septum primum and the septum secundum, that allows the two atria to communicate. It tends to be closed by a membrane attached to both septa in adulthood. Sometimes this closure is purely functional and kept closed by difference in pressure between the atria which is normally higher on the left than on the right side. A RA to LA flow is only possible in case of reversal of the pressure difference opening the baffle.
The abnormality is sometimes associated with an aneurysm of the atrial septum.
The closure of the foramen ovale is firstly functional before becoming anatomical. This is why the prevalence of a persistence of a patent foramen ovale decreases with age and is often considered as nearly physiological in newborns.
In summary:
- in the normal newborn, one can observe:
- the presence of a minimal and inconsequential left to right shunt persisting for a few days or weeks prior to anatomical closure of the foramen ovale
- re-opening of the foramen ovale in case of pulmonary arterial hypertension: return to fetal circulation, diaphragmatic hernia
- the reappearance in certain circumstances (screaming) of an intermittent right to left shunt, responsible for transient attacks of cyanosis: cases have been described during coughing or bucking in infants under general anesthesia
- the disappearance from the outset of any passage of blood from one atrium to another;
- when a heart defect is present, the foramen ovale may remain open and be the site of:
- a right to left shunt when the malformation is sited on the right heart or pulmonary circulation, with pressure in the RA > LA, responsible for permanent cyanosis,
- a significant left-right shunt when the malformation is sited on the left heart or interventricular septum and strongly raises left atrial pressure. This is called a "forced foramen ovale".
The presence of a patent foramen ovale usually remains inconsequential in the long term. However, it promotes:
- paradoxical embolisms: by definition, an embolism is paradoxical when it originates in the venous circulation and its arrival point is arterial. It is possible only in case of a communication between the venous and the arterial circuits. In case of patent foramen ovale associated with hyperpressure in the right atrium, such communication can be established. The circumstances favoring an increase of pressure in the RA and the opening of the patent foramen ovale are a cruoric, gaseous or fatty embolism.
- some migraines: the presence of a permeable foramen ovale is 2 to 5 times more common in case of migraine preceded by an aura. The mechanism is discussed: abnormal passage to the brain of serotonin present in the venous circulation, platelet microembols. Percutaneous closure of PFO often leads to the disappearance of these migraines.
- the development of a platypnea-orthodeoxy syndrome (see this term)
- strokes in case of scuba diving with a too fast ascent: micro-emboli of nitrogen
The diagnosis of patent foramen ovale is echocardiographic:
- in newborns and infants, the diagnosis is relatively simple: presence of a discrete defect between two portions of the interauricular septum. They partially cover each other, like tiles on a roof. It is confirmed by showing a left-right (or right-left) shunt on color Doppler examination.
.jpg)
A : picture of a PFO (FOP) ; B : passage of bubbles of agitated NaCl from the right (OD) to the left atrium (OG)
- in adolescents or adults, the search for PFO is usually done in the aftermath of an embolic accident and the purpose of the examination is to highlight the possibility of the appearance of a right to left shunt at the auricular level. The presence of a PFO can be suspected by transesophageal two-dimensional imaging. It will be confirmed by the realization of a contrast ultrasound cardiac echography at the end of a Valsalva maneuver.
- contrast ultrasound cardiac echography consists of the intravenous injection of a stirred 0.9 % saline solution. This modifies the echographic properties of the circulating blood which appears as countless micro-bubbles, the progression of which can be monitored, through the interatrial septum and in the left chambers of the heart if there is a right to left shunt.
- the Valsalva maneuver is practiced to transiently increase the pressures in the RA (displacement of the septum towards the LA) at its release and thus create the conditions for the appearance of a right-left shunt if a PFO is present.
Anesthetic implications:
- newborn: even if the cardiac ultrasound is normal, reopening of the foramen ovale is possible if the pressure in the RA becomes greater than in the LA
- laparoscopic surgery: the presence of PFO increases the risk of paradoxical air embolism
- neurosurgery: preoperative ultrasound. The presence of PFO is a contraindication to the sitting or elevated head position.
- postoperative ischemic stroke: there is a strong association between the presence of PFO (or ASD) and the onset of stroke within 30 days postoperatively, even after non-cardiac surgery. It is therefore necessary to look for the presence of a PFO in these cases.
References:
- Moorthy SS, Dierdorf SF, Krishna G, Caldwell RL, Alcorn DM.
Transient hypoxemia from a transient right-to-left shunt in a child during emergence from anesthesia.
Anesthesiology 1987; 66:234-5.
- Moorthy SS, Haselby KA, Caldwell RL, West KW, Albrecht T, France LW, Powell JC.
Transient right-left shunt during emergence from anesthesia: demonstration by color Doppler mapping.
Anesth Analg 1989; 68:820-2.
- Sukernik MR, Mets B, Bennett-Guerrero E.
Patent Foramen Ovale and its significance in the perioperative period.
Anesth Analg 2001 ; 93 : 1137-46.
- Rais G, Vassallo P, Schorer R, Bollen Pinto B, Putzu A.
Patent foramen ovale and perioperative stroke in noncardiac surgery: a systematic review and meta-analysis.
Br J Anaesth 2022 ; 129 : 898-908.
Updated: January 2023