It is by definition, the compression of the left renal vein between the superior mesenteric artery and the aorta. This causes a decrease in blood flow from the left renal vein to the inferior vena cava. It occurs slightly more commonly in women, staring in childhood with a peak frequency in young or middle aged women (20 to 40 years).
There are two types of the nutcracker syndrome:
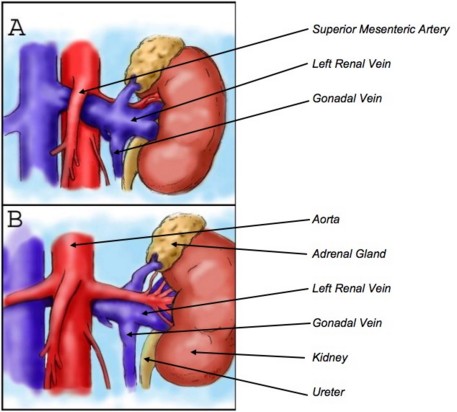
- the most classic one is the anterior form: the left renal vein is compressed between the superior mesenteric artery and the aorta (fig. A)
- the other rarer form is the posterior form: the left renal vein is compressed between the aorta and the vertebral body when the vein follows a retro-aortic path (fig. B)
Both types can be exceptionally combined in case of duplication of the left renal vein.
The clinical manifestations are linked by the consequences of venous stasis, upstream of the left renal vein:
- asymptomatic microscopic hematuria,
- macroscopic hematuria,
- abdominal pain or pain in the left flank, sometimes accompanied by nausea or vomiting,
- orthostatic proteinuria.
Venous stasis in the left gonadal vein can induce a pelvic pain syndrome, exacerbated by the sitting or standing position:
- in women: pelvic congestion syndrome often associated with pelvic varicose veins with dysuria, dyspareunia, dysmenorrhea,.
- in men: left varicocele with testicular pain.
Imaging usually shows a locatisd narrowing of left renal vein between the aorta and the superior mesenteric artery with an upstream dilation of the vein in direction of the renal hilum and of the homolateral gonadal vessels.
The term of 'Nutcracker syndrome' should be reserved for patients with clinical symptoms and signs associated with this anatomical feature because there are similar anatomical variants that have no clinical repercussion and should be in these cases rather called 'Nutcracker phenomenon'.
Conservative treatment is recommended in case of moderate hematuria. Before 18 years of age, the best option is a 'wait and see' attitude for at least two years because 75 % of patients will have spontaneous resolution of hematuria. The conversion enzyme inhibitors may improve orthostatic proteinuria.
When the symptoms are persisting or severe, some other treatments are possible:
- median nephropexy with excision of renal veins,
- bypass or transposition of the left renal vein
- transposition of the superior mesenteric artery
- renal autotransplantation, or even nephrectomy.
- stenting or embolization with coils of the pelvic varicose veins
Anesthetic implications:
check the hemoglobin level; possibly hemorrhagic pelvic surgery (venous congection)
References:
- Patel B, Samuel S.
Nutcracker syndrome - an unusual cause of chronic left upper abdominal pain : a case report.
A&A Practice 2019; 12: 69-72.
- Nalcacioglu H, Bilgici MC, Tekcan D, Genc G et al.
Nutcracker syndrome in children : role of doppler ultrasonographic indices in detecting the pattern of symptoms.
J Clin Med 2018; 7: doi: 10.3390/jcm7080214
- Alonso V, Sanchez-Abuin A, Velasco JJ, Marungan de Miguelsanz JM.
Pelvic congestion syndrome secondary to a circumaortic left renal vein.
J Pediatr 2020 ; 220 : 261-2
Updated: June 2020