(Wilms tumor)
Represents 5-14 % of all solid tumors and 90 % of renal tumors in children. The peak frequency is around 3-4 years of age, regardless of gender. Bilateral forms concern 5.6 % of cases. A heterolateral nephroblastoma occurs in 1 to 3 % of the successfully operated first tumors.
Different forms have been identified:
- sporadic: the vast majority of cases,
WT1 [MIM 194 070]: mutation of the WT1 gene (11p13), or, more rarely, of the BRACA2 gene (13q13.1) or somatic mutation of the GPC3 gene (Xq26 .2) or the WTX gene (Xq11.2)
WT2 [MIM 194 071]: mutation of the ICR1 gene (11p15.5)
WT3 [MIM 194 090]: mutation in 16q
WT4 [MIM 601 363]: mutation in 17q12-q21
WT5 [MIM 601 583]: mutation of the POU6F2 gene (7p14)
WT6 [MIM 616 806]: mutation of the REST gene (4q12)
- familial (1.5 % of cases): these forms are associated with mutations of the FWT-1 (17q) or FWT-2 (19q) genes
- syndromic, (about 10 % of cases), which are categorized into two groups depending on whether or not there is an associated body hypertrophy.
The main syndromic forms with body hypertrophy are:
- Beckwith-Wiedemann syndrome (10-20 % of them develop nephroblastoma); mutation of the ICR1 gene (11p15.5)
- body hemihypertrophy (3 to 5 % of them develop nephroblastoma)
- Sotos syndrome or cerebral gigantism: mutations of the NSD1 gene (5q35); there are a few rare not NSD1 forms
- Perlman syndrome, a combination of facial dysmorphism, gigantism, renal dysplasia (hamartomas) and islet of Langerhans hyperplasia;
- Simpson-Golabi-Behemel syndrome (somatic mutation of the GPC3 gene (Xq26.2)), phenotypically similar to Beckwith-Wiedemann syndrome.
The main syndromic forms without body hypertrophy are:
- congenital aniridia;
- Denys-Drash syndrome, which combines pseudohermaphrodism, nephropathy with nephrotic syndrome and gonadoblastoma: WT-1 gene (11p13);
- WAGR syndrome (acronym for "Wilms tumor, Aniridia, Genito-urinary abnormalities or Gonadoblastoma, and mental Retardation" where a nephroblastoma is associated with aniridia, urogenital malformations and mental retardation; gene WT-1 (11p13)
- Down's syndrome.
Half of the children with a mutation of the WT1 gene also carry mutations of the CTNNB1 gene coding for beta-catenin.
The tumor develops from the fetal metanephrotic blastema. The degree of cell maturation is correlated with prognosis: there are three different groups of histological forms (low, intermediate or high risk) that allow the post-operative treatment to be adapted. There is a rhabdomyomatous form (10 %) that affects younger children.
Clinical presentation:
- large abdominal mass with sometimes considerable increase in abdominal girth,
- abdominal pain in only 1/3 of cases,
- anemia, fever, hematuria
- systemic hypertension is observed in 1/3 of cases: it is due to the secretion of renin either by tumor tissue or secondary to the compression of the renal artery.
- chemosensitive pulmonary metastases are often present (90 %) at the initial check-up; hepatic (15 %), abdominal (5 %), osseous (4 %) or lymph nodes (4 %) metastases can also be present.
Approximately 8 % of these cases of nephroblastoma are associated with an acquired paraneoplastic von Willebrand type syndrome: it is generally a biological abnormality with no clinical impact but cases of hemorrhagic diathesis have been described. It is therefore important to check the hemostasis before surgery.
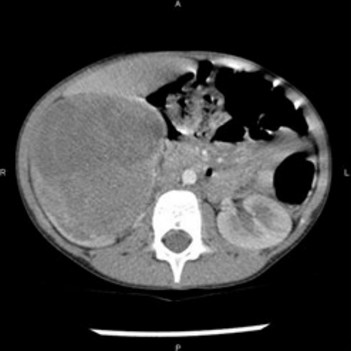
Abdominal echography confirms the presence of a large solid mass of renal origin and should identify its venous drainage, and look for a possible thrombus in the renal vein that extend up to the right atrium. The severity grade is based on MRI and CTscan data.
Extrarenal locations can develop from metanephros remnants: they are more common in the retroperitoneal space but uterine, ovarian, inguinal and thoracic locations have been described. The retroperitoneal forms can cause spinal cord compression by invasion of the vertebral spinal canal ('hourglass' type tumor).
|
severity |
characteristics |
survival at 5 yrs |
|
Grade 1 |
the tumor is limited to the renal capsule and is completely resected surgically |
95 % |
|
Grade 2 |
the tumor presents an extra-renal extension and can be completely resected surgically |
> 90 % |
|
Grade 3 |
incomplete resection of the tumor, without metastases |
< 60 % |
|
Grade 4 |
presence of metastases of hematogenic origin |
< 10 % |
|
Grade 5 |
bilateral tumor |
0 % |
Wilms Tumor Severity Classification
In Europe, the therapeutic strategy is: chemotherapy (Actinomycin D and vincristine), surgery and then chemotherapy with or without radiotherapy.
The surgical approach consists in a wide transverse abdominal incision (or robotic surgery) to identify and isolate the renal pedicle. The tumour is usually large and fragile. The dissection is extensive, difficult, time-consuming and hemorrhagic.
In case of invasion of the inferior vena cava or of the R.A. it may be necessary to perform the intervention under cardiac bypass..
The very large tumors sometimes require preoperative chemotherapy to reduce their size, decrease the size of the thrombus in the renal vein (or even to make it disappear) but it can complicate the surgical follow-up and severely interfere with healing.
Anesthetic implications:
The presence of a major abdominal tumour produces various consequences : a reduced diaphragmatic excursion, compression of IVC and delayed gastric emptying.
Preoperative: control of total blood count and hemostasis (paraneoplastic syndrome?), echocardiography (chemotherapy, side effects of high BP) to assess myocardial function;
Monitoring: invasive monitoring of blood pressure, a central venous catheter, a bladder catheter. It is better to insert the IV catheters in the upper limbs so that effective vascular filling can be provided even in case of IVC cross-clamping. Prevention of hypothermia.
In the absence of hemostatic disorders, it is useful to associate an epidural block with general anesthesia. The risk-benefit ratio of the technique must be individualized because the presence of an abdominal tumor leads to an increased risk of venous effraction (collateral circulation through the epidural venous network) and major hypotension when the increased sympathetic tone that counterbalances the compression of the inferior vena cava is abolished by the sympathetic bloc (supine hypotensive syndrome as during the last trimester of pregnancy). In some cases, it is wise to perform the epidural injection of LA only when the tumor has been removed. It is also important to ensure that there are no vertebral metastases or tumor invasion of the vertebral canal. The neurotoxicity of vincristine should also be kept in mind.
References :
- Przybylo HJ, Stevenson GW, Backer C, Luck SR, Webb CL, Morgan E, Hal SC.
Anesthetic management of children with intracardiac extension of abdominal tumors.
Anesth Analg 1994; 78:172-5.
- Poerink-Stockschlader ABJ, Dekker I, Risseuw-Appel IM, Hahlen K.
Acquired von Willebrand disease in children with Wilms tumor.
Medical and Pediatric Oncology 1996 ; 26 :238-43.
- Cojean N, Entz-Werle N, Eyer D, Becmeur F, Kehrli P, Marcellin L, Christmann D, Babin A, Lutz P.
Néphroblastome en sablier: une cause inhabituelle de compression médullaire.
Arch Pédiatr 2003 ; 10:1075-8.
- Whyte SD, Ansermino JM.
Anesthetic considerations in the management of Wilms tumor.
Pediatr Anesth 2006; 16:504-13.
- Baxter PA, Nuchtern JG, Guillerman RP, Mahoney DH t al.
Acquired von Willebrand syndrome and Wilms tumor : not always benign.
Pediatr Blood Cancer 2009 ; 52 :392-4
- Granger J, Gidvani VK.
Acquired Factor VII deficiency associated with Wilms tumor.
Pediatr Blood Cancer 2009 ; 52 :394-5
- Sarhan OM, El-Baz M, Sarhan MM, Ghali AM, Ghoneim MA.
Bilateral Wilms' tumors: single-center experience with 22 cases and literature review.
Urology 2010; 76:946-51.
- Martínez CH, Dave S, Izawa J.
Wilms' tumor.
Adv Exp Med Biol 2010; 685:196-209.
- Miura H, Kawana S, Sugino S, Kikuchi C, Yamauchi M.
Successful management of an infant with hypertensive heart failure associated with Wilms tumor : a case report.
JA Clinical Reports 2020 ; 6 :12, doi/10.1186/s40981-020-00318-7
Updated: February 2021