(Spinal dysraphism, spina bifida)
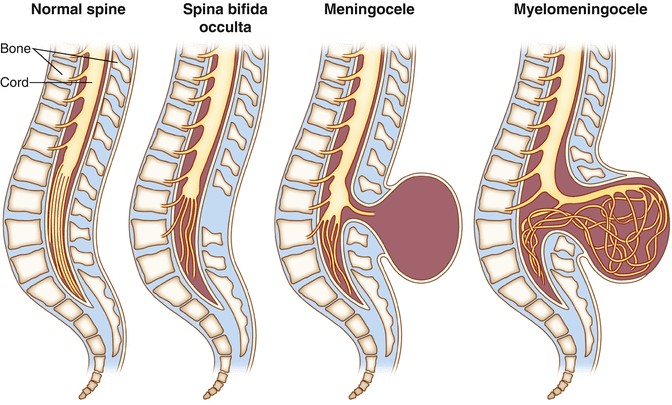
The spinal dysraphisms are usually categorized in two major clinical groups that only MRI allows to properly analyze and classify:
- "open" dysraphisms or spinal myelodysplasias: leptomeningeal and sometimes nerve structures are directly exposed to the external environment: myelomeningoceles, myeloschisis, hemimyelomeningoceles, hemimyeloceles; These dysraphisms are always associated with an Arnold Chiari type II malformation (see this term).
- « covered » dysraphisms or spinal myelodysplasias: they are covered with intact skin but easily identifiable by their dystrophic aspect
There are 2 subgroups:
o dysraphism with a lipomatous subcutaneous mass, including: lipomyeloschisis, lipomyelomeningoceles, meningoceles and myelocystoceles; children affected by a myelocystocele frequently have associated abdominal wall abnormalities reflecting a more severe involvement and with a significantly more negative neurological prognosis;
o massless dysraphism, including different forms of pure dysraphism: more or less extended dorsal neurenteric fistulas, neurenteric cysts, divided and fixed medulla (diastematomyelia: see this term), dermal sinus, caudal regression, segmental spinal dysgenesis, narrow filum terminale, intradural lipomas, persistent terminal ventricle.
The severity of the lesions is variable, ranging from obvious externalized forms to occult forms (spina bifida occulta) which may be ignored for a long time and discovered fortuitously later in life (if ever). Skin anomalies located on the axis of the spinal processes at the level of the lumbosacral region should be considered as a sign of an underlying spinal anomaly e.g., a fixed medulla.
Anesthetic implications:
Skin anomalies located on the spinal processes line at the level of the lumbar region should be regarded as suspect, particularly of an underlying tethered spinal cord. Regional echography during the neonatal period often allows the detection of concealed anomalies. A MRI is indicated for an accurate diagnosis.
Treatment of open dysraphism: emergency neonatal surgery if CSF is leaking or if the membrane covering the mass is damaged. Surgery is performed in the prone position. Sometimes positioning for the induction of anesthesia can be difficult : you can for example place the lumbosacral mass on in a head support.
It is indeed important to avoid compressing the site of dysraphism to avoid:
- any damage to or infection of the nervous structures if the covering membrane is open
- intracranial hypertension by compressing the CSF inside the mass which, in that case, can thus quickly be pushed to the central nervous cavities of the newborn. This complication has been described in adults.
Surgery may be hemorrhagic: blood grouping and RAI (search for irregular agglutinins) should be obtained before surgery. Risk of hypothermia. Myorelaxants should be avoided to allow the surgeon to evaluate the neurological function during surgery (stimulation of the nerve roots present in the myelomeningocele). Patients are extubed fully awake after checking the absence of apneas, the stability of the hemodynamic parameters and that body temperature is normal.
Some teams have described the injection of local anesthetic into the lumbar or sacral myelomeningocele to allow its closure under 'spinal anesthesia'.
Primary prevention of latex allergy: avoid any latex-containing equipment.

References :
- Kaufman BA.
Neural tube defects.
Pediatr Clin North Am 2004; 51:389-419.
- Tortori-Donati P, Rossi A, Biancheri R, Cama A.
Magnetic resonance imaging of spinal dysraphism.
op Magn Reson Imaging 2001; 12:375-409.
- Rossi A, Biancheri R, Cama A, Piatelli G, Ravegnani M, Tortori-Donati P.
Imaging in spine and spinal cord malformations.
Eur J Radiol 2004; 50:177-200.
- Northrup H, Volcik KA.
Spina bifida and other neural tube defects.
Curr Probl Pediatr 2000; 30:313-32.
- Viscomi CM, Abajian JC, Wald SL, Rathmell JP, Wilson JT.
Spinal anesthesia for repair of myelomeningocele.
Anesth Analg 1995; 81:492-5.
- Drummond JC, Ciacci JD, Lee RR.
Direct pressure on a pseudomeningocele resulting in intraoperative cerebral ischemia.
Can J Anesth 2014; 61: 656-9.
Updated: February 2019