Prevalence: 1/300,000 but much more frequent in Asia, especially Japan. Moya Moya disease has two peaks in frequency: between 5 and 15 years of age, and between 30 and 40 years of age. Girls appear to be affected more often than boys. Cerebral arteriopathy of unknown origin, characterized by progressive occlusion of intracranial carotid vessels and/or proximal branches of the anterior and middle cerebral arteries, and development of collateral circulation from leptomeningeal vessels and other extra- and intracranial branches of the carotid arteries. Angiography of the collateral network resembles a puff of smoke, giving the condition its name (moyamoya in Japanese).
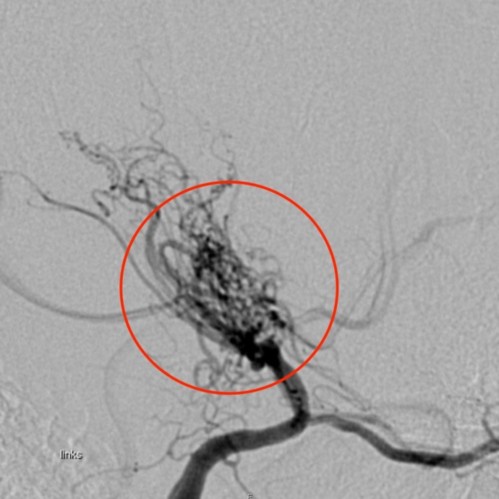
Source: Inselspital Bern
Histology: progressive obliteration of the lumen by thickening of the intima (hyperproliferation of its components and angiogenesis), with reduction in vessel outer diameter and thinning of the media. The wall of collateral vessels is fragile and can be the source of microaneurysms.
The pathophysiology is complex (aberrant angiogenesis preceding stenosis or vice versa?) and undoubtedly different in children and adults.
A distinction is made between
- Moya-Moya disease, which is isolated and idiopathic, There are genes whose variants predispose to Moya-Moya disease. These genetic forms, of autosomal recessive or dominant transmission, are rare (2 to 10 % of cases) and divided into:
* MYMY 1: MYMY1 locus (3p26-p24.2 [MIM 252 350])
* MYMY 2: RNF213 gene (17q25) [MIM 607 151].
* MYMY 3: MYMY3 locus in 8q23 [MIM 608 796]
* MYMY 4: X-linked transmission, MYMY4 locus in Xq28 [MIM 300 845]: short stature, hypergonadotrophic hypogonadism, facial dysmorphia (moderate ptosis and retrognathia), and dilated cardiomyopathy in one case.
* MYMY 5: ACTA2 gene (10q23) [MIM 614 042].
* MYMY 6: GUCY1A3 gene (4q32), associated with esophageal achalasia [MIM 615 750].
* MYMY 7: ANO1 gene (11q13) [MIM 620 687].
- Moya-Moya syndrome, where the arteriopathy is associated with another pathology such as: trisomy 21, neurofibromatosis type 1, Alagille syndrome, sickle cell anemia, Marfan syndrome, Fanconi anemia, hyperthyroidism.
There are also cases of acquired Moyamoya syndrome following brain irradiation or bacterial meningitis.
Angiographic staging according to Suzuki:
|
Grade I |
carotid artery stenosis without collateral circulation |
|
Grade II |
presence of collateral vessels at the level of the basal ganglia |
|
Grade III |
very important collateral vessels |
|
Grade IV |
stenosis or occlusion at the level of the circle of Willis and
|
|
Grade V |
network of extracranial collaterals |
|
Grade VI |
total occlusion of the carotid artery |
Clinical signs:
- repeated ischemic (transient ischemic hemiplegias or successive hemiparesias) and/or hemorrhagic attacks: it is the cause of about 6 % of strokes of the child. Ischemic attacks are typically caused by hyperpnea or emotions: hypocapnia causes vasoconstriction of the collateral vessels already dilated to compensate chronic ischemia.
- chronic cerebral circulatory insufficiency: headache, epilepsy
- renal artery stenosis is sometimes associated.
Treatment :
Medical: antiplatelet agents (aspirin), sometimes calcium channel blockers
Surgical: surgical anastomoses between intra - and extracranial circulations.
These anastomoses are:
- either direct (superficial temporal artery => to middle cerebral artery) the effect of which is immediate
- or indirect, the results of which are progressive: 1) anastomosis of the temporalis muscle on the pia-mater or the underlying dura-mater, 2) multiple bur holes to put the vascularization of the scalp and the meninges contact ...
Anesthetic implications:
the priority is to maintain a normal cerebral blood flow and perfusion pressure, and to avoid any cause of cerebral ischemia:
- aiming at normocapnia: because hypocapnia = vasoconstriction of healthy vessels and decrease in flow in both the collateral and diseased vessels. Hypercapnia = dilation of healthy vessels and subsequent « steal » to non-ischemic areas.
- avoidance of large BP variations (intubation, overdose...): maintain the mean arterial pressure in a range of ± 15 % of normal values
- in case of cranial surgery, propofol-based TIVA seems preferable to sevoflurane
- prevent hypovolemia: administer 20 ml/kg of crystalloids at induction and provide IV fluids for maintenance with 1.5 times the 4-2-1 rule
- prevent pain and crying (induction, alarm clock, care). No contraindication to regional anesthesia (aspirin. )
- avoidance of hypo- and hyperthermia.
- spinal anesthesia and epidural analgesia (obstetrics) have been used successfully.
NIRS monitoring with measurement of baseline values before induction. Keeping in mind the limits of the technique, measuring NIRS at baseline (before induction) and its changes under anesthesia could help determine the limits of cerebral autoregulation and thus determine the ideal mean systemic arterial pressure for each patient. The risk of cerebral complications after anesthesia for a non-neurosurgical procedure is estimated to about 1 %.
References :
- Yasukawa M, Yasukawa K, Akagawa S, Nakagawa Y, Miyasaka K.
Convulsions and temporary hemiparesis following spinal anesthesia in a child with MoyaMoya disease (lettre).
Anesthesiology 1988; 69: 1023-4.
- Parray T, Martin TW, Siddiqui S.
Moyamoya disease: a review of the disease and anesthetic management.
J Neurosurg Anesthesiol 2011; 23:100-9. - Jabbour H, Jabbour K, Ayoub EN,Yazbeck P, Antakly M-C.
Rachianesthésie chez un patient connu avoir une maladie de Moya Moya.
Annales Françaises d’Anesthésie et de Réanimation 2004 ; 23 : 505-7 - Baykan N, Ozgen S, Ustalar S, Dagçinar A, Ozek MM.
Moyamoya disease and anesthesia.
Pediatr Anesth 2005; 15: 1111-5. - Ibrahimi DM, Tamargo RJ, Ahn AS.
Moyamoya disease in children.
Childs Nerv Syst 2010 ; 26 : 1297-1308. - Lee JK, Williams M, Jennings JM, Jamrogowicz JL, Larson AC, Jordan LC, Heitmiller ES, Hogue CW, Ahn ES.
Cerebral autoregulation in pediatric moyamoya disease.
Pediatr Anesth 2013; 23: 547-56. - Bang OY, Fujimura M, Kim S-K.
The pathophysiology of Moyamoya disease: an update.
Journal of Stroke 2016;18:12-20 doi.org/10.5853/jos.2015.01760 - Lee GY, Kim CH, Chung RK, Han JI.
Intracranial hemorrhage during laparoscopic cholecystectomy due to unrecognized moyamoya disease.
J Clin Anesth 2015; 27: 81. - Giustini AJ, Stone AS, Ramamoorthy C.
Moyamoya disease in children and its anesthetic implications : a review.
Pediatr Anesth 2020; 30 :1191-8. - Lang S-S, Vollmer E, Wu L, Bathini A, Kanuga B et al.
A retrospective study of neurological complications in pediatric patients with moyamoya disease undergoing general anestthesia.
Anesth Analg 2021; 132:493-9.
Updated: December 2024