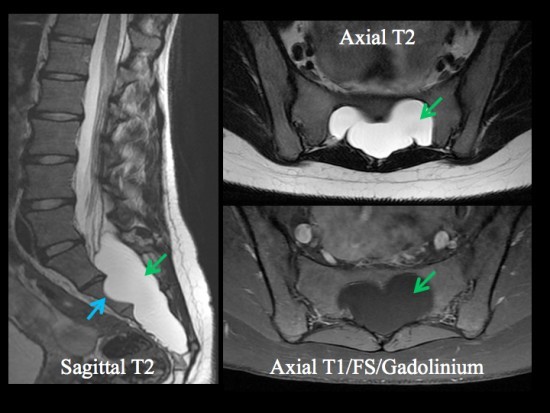
(Perineural cyst, extra-dural arachnoid cyst)Annual incidence estimated at 5% but the incidence of the symptomatic forms is less than 1/2,000. Extradural cyst at the level of the sheath of a nerve root : it is formed by the outgrowth of the arachnoid or dura mater which constitutes a pocket containing cerebrospinal fluid. The wall of the cyst contains nerves or ganglion cells. This type of cyst is most often found in the sacral area (S2 and S3), rarely at other levels of the spine. This pathology is more common in women than in men.
Possible symptoms: radiculopathy, pain when coughing, paresthesia, sphincter or sexual dysfunction... The rupture of the cyst may cause spontaneous intracranial hypotension (see this topic).
Causes:
- congenital
- traumatic: carrying heavy loads
Diagnosis: scanner, CT scan, MRI, myelography, sometimes ultrasound.
There are 3 types of perimedullar cysts:
- type I: extradural, of congenital origin and containing no nerve tissue. It is a minor form of sacral meningocele; frequent association with other congenital anomalies: teratomas, dermoid, genitourinary or anorectal abnormalities.
- type II: extradural, often multiple and containing nervous tissue. This is the true Tarlov cyst, located posteriorly or on the side of the nerve root. A variant is the meningeal diverticle which is located in front the the root nerve and communicates with the subarachnoid space.
- type III: intradural: in general at the thoracic level behind the medulla if congenital, anterior to it if acquired.
Differential diagnosis: meningeal cysts. These fill up directly during myelography while peri-radicular cysts fill up more slowly.
Treatment: only in very symptomatic cases: drainage, laminectomy, excision
Anesthetic implications:
increased risk of subarachnoid breach in case of neuraxial block; a blood patch can be tried in case of postural headaches possibly caused by the rupture of a cyst (fall, coughing, ..)
References :
- Schievink WI, Maya MM, Mouy C, Moser FG, Sloninsky L.
Spontaneous intracranial hypotension in childhood and adolescence.
J Pediatr 2013 ; 163 : 504-10
- Arora V, Rozet I.
Tarlov cysts: incidental finding during subarachnoid drain placement.
Anesthesiology 2016; 125: 598
- Qasem F, McCallum C, Armstrong P.
Epidural blood patch treatment for headache caused by a ruptured Tarlov cyst.
Can J Anesth 2017; 64: 983-4.
Updated: September 2017*