Heterogeneous group of pathologies characterized by skin xerosis (dry, thin and fragile skin) and excessive peeling (aspect
of scales). Comes from ichtyus which means fish scale in greek.
Ichthyosis vulgaris is the most frequent (1/300). It is not visible at birth but appears after a few months: there are fine greyish scales on the trunk and the extension surfaces of the limbs with accentuation of the palmoplantar creases. It affects both sexes. There is no itching. It is sometimes associated with eczema. It improves in the summer, thanks to the sun.With regard to congenital ichthyosis, there are:
- isolated ichthyosis
1) non-bullous
- X-linked ichthyosis (1/2,000): deficiency in steroid sulfatase (STS gene); only the boys are affected; fine peeling at birth following later by large, dark brown scales on the trunk and limbs; hyperkeratosis of the face of extension surface of the joints ("black ichthyosis") can produce a dirty appearance, especially at the level of the neck. Corneal opacities, cryptorchidism is common.
- congenital ichthyosis with autosomal recessive transmission (1/200,000): in 30% of cases, mutations in the TGM1 gene (transglutaminase 1 keratinocytes) on 14q11. Other genes have been identified (see below). Onset at birth: generally as a collodion baby, sometimes as an ichthyosiform erythroderma. Ichthyosis Congenita prematurity syndrome (SLC27A4 gene) belongs to this category.
The course is then variable:
a) either lamellar Ichthyosis: (genes: TGM1, ABCA12, ALOX12B, NIPAL4) large scales of dark brown color and adherent everywhere on the body, little or no erythroderma; ectropion and eclabion (eversed lips), alopecia, yellow palmoplantar keratoderma and hyperkeratosis of the elbows and knees;
b) or ichthyosiform bullous congenital erythroderma (genes: ALOX12B, ALOXE3 TGM1, ABCA12, CYP4F22, NIPAL4): erythroderma covered with small whitish scales.
- collodion baby with spontaneous healing (Self Healing Collodion Baby): (genes: TGM1)
ALOX12B or ALOXE3): collodion baby at birth but full healing during the first 3 months of life.
2) bullous ichthyosis
- congenital bullous ichthyosiform erythroderma (1/300,000): autosomal dominant transmission; at least 6 different phenotypes. At birth, appearance of widespread burn (DD: Epidermolysis Bullosa). Later, erythroderma covered with flabby bubbles with skin scaling and risk of superinfection; around 3-4 years, the bubbles diminish in number and an inhomogeneous, brown yellow color hyperkeratosis appears ("snake skin"). This hyperkeratosis favors bacterial infection and is thus responsible for a foul odor.
- Siemens ichthyosis bullosa: very rare; autosomal dominant transmission (KRT1 or KRT10 genes); no or moderate erythroderma; fragility of the skin that causes small bullous detachments following local in trauma ("exfoliative scaling") in childhood and limited hyperkeratosis limited to the areas of skin stress in adults.
- ichthyosis associated with extracutaneous or syndromic signs:
1) Netherton syndrome, see Netherton, syndrome of
2) trichothiodystrophy (see this term) autosomal recessive transmission; sulfur amino acid deficiency; baby collodion and severe ichthyosis with palmoplantar hyperkeratosis and nail dystrophy, partial alopecia and absence of ectropion; mental and growth retardation, hypogonadism; susceptibility to infection
3) autosomal recessive ichthyosis with hypotrichosis: very rare; autosomal recessive transmission of mutations in the ST14 gene; sometimes baby collodion followed with non-inflammatory ichthyosis with hypotrichosis that spares the face; scattered, fragile, dry and thin hair that grows slowly; sometimes photophobia with corneal opacities and dental anomalies.
4) Sjögren-Larsson syndrome: see Sjögren-Larsson, syndrome
5) Keratitis Ichtyosis Deafness (KID) syndrome: see KID syndrome
6) Ichtyosis follicularis alopecia and photophobia (IFAP) syndrome: rare; probably X-linked recessive transmission; association of a congenital follicular ichthyosis, alopecia (hair, eyelashes and eyebrows) and photophobia; ichthyosis predominates on the scalp and the extension surface of the limbs (sandpaper appearance).
7) Chanarin-Dorfman syndrome: see Dorfman-Chanarin disease, syndrome of
8) Gaucher disease: see Gaucher, disease of : a subgroup of children suffering from type II presents an acute evolution with hydrops and congenital ichthyosis; early death in the neonatal period.
9) Neu-Laxova syndrome: see Neu-Laxova syndrome of
10) NISCH, syndrome see NISCH
11) ARC syndrome, see ARC
(12) Conradi-Hünermann syndrome, see Conradi-Hünermann
Rud syndrome (X-linked or autosomal recessive transmission) which combines ichthyosis, mental retardation with epilepsy, short stature, hypogonadism and polyneuropathy, is currently reclassified in several of the above described syndromes.
Two clinical pictures at birth:
- collodion baby (see this term): the infant is completely covered with a fibrous membrane at birth; this membrane cracks and disappears within a few weeks. Significant mortality and morbidity: hypothermia, superinfection, hypernatremic dehydration. The skin later becomes normal or ichthyosiform. Evolution: 48% to congenital ichthyosiform erythroderma, 12% to lamellar ichthyosis, 10% to ichthyosis vulgaris, 10% to normal skin.
- Harlequin fetus : the most severe form of congenital ichthyosis; autosomal recessive transmission of mutations in the ABCA12 gene; the newborn was born enclosed in thick and wide scales separated by red cracks. A significant stress is applied to the skin which causes: ectropion, eclabion, eversion of the ears and nose. The extremities get swollen by the tourniquet effect caused by thickening of the skin. Early death from respiratory or infectious complications.
.jpg)
Treatment: symptomatic, locally: hydrating and keratolytic solutions (in case of hyperkeratosis). Sometimes, immunosuppressant treatment, either local or systemic.
Anesthetic implications:
according to the importance and extent of ichthyosis:
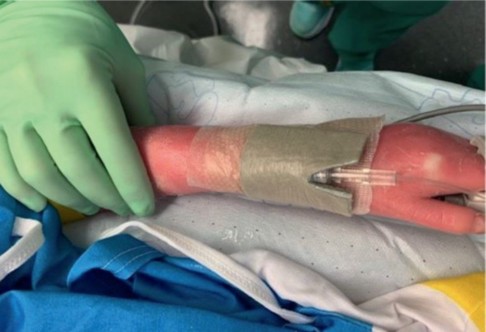
- ichthyosis vulgaris: difficulty of securing intravenous catheters and monitoring electrodes; increased risk of local infection in case of percutaneous catheters (IV, RA)?
- congenital ichthyosis: difficult peripheral venous access, difficulties to secure catheters and tracheal tubes as hyperkeratosis decreases the stickiness of dressings, risk of skin surinfection, eyes protection.
.jpg)
References :
- Chiavérini C.
Ichtyoses génétiques.
Ann Dermatol Vénéréol 2009 ; 136 : 923-34. - Rado R, Ellis LZ, Gamble R, Funk T et al.
Collodion baby : an update with a focus on practical management.
J Am Acad Dermatol 2012; 67: 1362-74. - Craiglow BG.
Ichthyosis in the newborn.
Sem Perinatol 2013; 37: 26-31. - Smart KJ, Gruffi CA, Doherty TM.
Anesthetic management of a patient with Harlequin ichtyosis.
Case Reports in Anesthesiology 2021 doi/10.1155/2021/9953320
Updated: August 2021