(hepatoblastoma, hepatocarcinoma, undifferentiated embryonic sarcoma, hamartoma, hemangioendothelioma, nodular focal hyperplasia, adenoma)
1) hepatoblastoma [MIM 114 550]
It represents 1 to 2 % of the malignancies in childhood. Somatic mutation of the APC gene (5q22.2). Tumor of embryonic origin that mainly affects children under 2 years of age.
It is often associated with a somatic malformation such as:
- Beckwitt-Wiedemann syndrome
- hemihypetrophy of the body.
The risk factors include preterm birth (birth weight < 1500 g), familial rectocolic polyposis, smoking during pregnancy, and preeclampsia. But also: Li Fraumeni syndrome (see this term) or trisomy 18.
The signs are usually a paucisymptomatic abdominal mass discovered by chance. Pain and jaundice are rare. A clinical presentation of intratumoral hemorrhage or intraperitoneal rupture (in case of trauma) is exceptional.
A major increase in serum alpha-fetoprotein level is observed in 75 % of cases. There may be lung metastases.
Two paraneoplastic syndromes are sometimes observed:
- thrombocytosis, by secretion of thrombopoietin;
- precocious pseudopuberty, by secretion of HCG.
According to the tumoral histology, one distinguishes:
- purely epithelial forms (the majority of cases)
- mixed epithelial and mesenchymatous forms and, depending on the epithelial contingent, four histological types are individualized: fetal, embryonic, small cells either undifferentiated or macrotrabecular.
The treatment consists of several chemotherapies (cisplatin, doxorubicin) followed by surgical resection or liver transplantation if the tumour is not resectable.
2) hepatocarcinoma: [MIM 114 550]
Rare tumor in children. Its frequency increases with age. Somatic mutation of the CASP8 (2p33.1), CTNNB1 (3p22.1), PIK3CA (3q26.32, MET (7q31.2), CEOFRL (8p22), AXIN1 (16p13.3) or TP53 (17p13.1) genes. It sometimes occurs on a cirrhotic context: hepatitis B or C, tyrosinemia I, glycogenosis Ia (see these terms).
The signs usually consist of a painful abdominal mass with altered general condition. The increase in the serum alpha-fetoprotein level is less frequent and less elevated than in case of hepatoblastoma.
Two paraneoplastic syndromes can be observed:
- polycythemia
- feminization in boys.
The prognosis is worse than in case of hepatoblastoma and chemotherapy is less effective. Treatment consists of surgical resection or liver transplantation if the tumour is not resectable.
3) fibrolamellar hepatocarcinoma
Rare: represents 1 to 9 % of the liver tumors. It is a histological variant of hepatocarcinoma, which develops very slowly on a healthy liver. Tumor cells express massive quantities of the chimeric DNAJB1-PRKACA protein following a deletion in chromosome 19. Blood levels of transcobalamine I and or II are high, which allows a tracking of the evolution of the tumor.
4) undifferentiated embryonic sarcoma
Rare tumor occurring mainly in 6 to 10 years old children. It is a cystic-looking abdominal mass. The prognosis is severe: frequent pulmonary, pleural and peritoneal metastases.
5) rhabdoid liver tumor [MIM 609 322, 613 325]
Very rare. Usually in infants or small children. Very aggressive sarcomatous tumor. Germinal mutation (autosomal dominant transmission of a familial predisposition to rhabdoid tumors) or somatic mutation of the SMARCB1 gene (22q11.23).
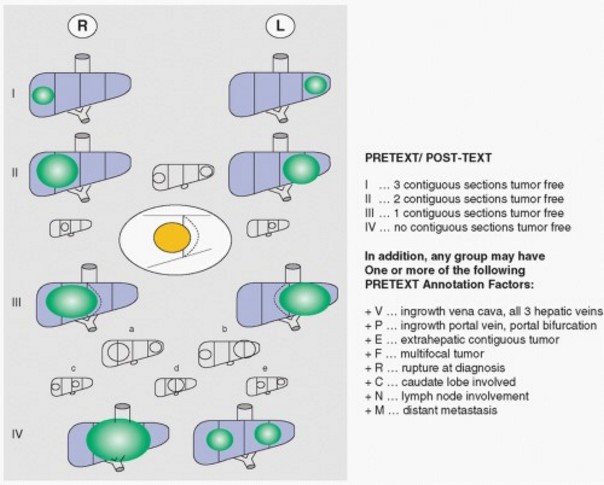
For those three types of malignant liver tumors, radiological imaging techniques allow a pre- and post-chemotherapy extension assessment based on the number of liver sections involved, vascular involvement, extrahepatic extension and the presence of metastases: the PRETEXT and POSTTEXT stages
stage I: the tumor affects only one liver section
stage II: the tumor affects two adjacent liver sections
stage III: the tumor affects three adjacent liver sections
stage IV: the tumor affects all four liver sections
The following items are used to adapt the staging:
- E = extra-hepatic extension of the tumor
- F = multifocal tumor
- M = metastases presence of distant metastases
- V = all 3 hepatic veins involved
- P = portal vein involved or its bifurcation
- C1 = caudal lobe involved (segment 1)
- R = tumor ruptured at the time of diagnosis
- N = lymph node involvement
Possible treatments: chemotherapy followed by a more or less extensive hepatectomy, chemoembolization of the tumor, preoperative embolization, liver transplantation.
6) mesenchymal hamartoma (von Meyenburg Complex Disease)
Represents about 8 % of the child's liver tumors. Benign solid tumor that usually appears before 2 years of age. It is associated with a mutation of the MALAT1 (11q13), C19MC (19q13.4) gene or, more rarely, with a germinal or somatic mutation of the DICER1 gene (14q32.13) (see this term). It is either appended to a liver lobe (figure) or well encapsulated inside the liver.
In case of multiple biliary microhamartomas located in the subcapsular zones, it is known as von Meyenburg complex : these lesions are benign and consist of small bile ducts within an hyaline fibrous stroma. They are often asymptomatic and require no treatment.

7) hemangio-endothelioma
Vascular tumor that appears during the first 6 months of life and has a growing phase of 6 to 8 months before stabilizing. It then starts a slow spontaneous regression process from 18 months-2 years of age to 6-8 years of age. It is a multifocal lesion often accompanied by skin lesions. It presents as hepatomegaly and can result in cardiac failure. Currently, propranolol (associated with corticosteroids or not) is used successfully at the 2 to 3.5 mg/kg/day dose. If possible, surgery (usually liver transplantation) is avoided, as it is very hemorrhagic and carries a risk of significant mortality and morbidity.
8) adenoma
Benign tumor, usually unique but that can be multiple ("hepatocellular adenomatosis") when it is a late complication of glycogenosis Ia (a malignant transformation is possible in case of somatic mutation of the IGF2R gene (6q25.3)), glycogenosis III (Cori's disease) or IV, and β-thalassemia. Risk factors : MODY 3 diabetes, congenital portosystemic fistula, use of anabolic androgens or oral contraceptives, familial adenomatous polyposis, Klinefelter syndrome.
Treatment: monitoring of the evolution, risk of malignant transformation (10 %).
9) nodular focal hyperplasia
Benign non-evolving tumor, more common in adolescents. It could be the result of localized hypervascularization of the liver. In adult women, it could be facilitated by oral contraception.
Anesthetic implications:
- in case of preoperative chemotherapy: check the blood count and the hemostasis but also ECG and echocardiography to assess the myocardial function.
- look at the preoperative examinations (ultrasound, CT-scan, sometimes cavography) to know the precise anatomy and vascularization of the tumor, and its relationship with the large vessels, in search of compression or invasion of the inferior vena cava (IVC).
- inhalatory or intravenous induction; use a cuffed endotracheal tube to avoid ventilatory problems when installing abdominal retractors. Maintenance is provided by controlled ventilation with PEEP using an O2/air mixture associated with isoflurane or sevoflurane and an opioid (fentanyl, sufentanil, repeated bolus or continuous infusion).
- the liver function is usually normal (except in case of pre-existing cirrhosis) and if there are no bleeding disorders, the combination of general anesthesia and a low thoracic epidural gives excellent results. It should be kept in mind, however, that in case of extensive hepatectomy, a more or less significant liver failure, with moderate hemostasis disorders and decreased metabolic capacity of the liver, is inevitable during the first postoperative days. The risk-benefit ratio of the technique must therefore be assessed individually.
- invasive monitoring to assess and compensate for the hemodynamic and metabolic consequences of the hepatectomy: invasive blood pressure measurement, central venous catheter, urinary catheter. It is better insert the peripheral venous access in the upper limbs so that vascular filling remains effective during IVC clamping. In the case of intravascular tumor extension (IVC or right atrium (RA), surgery is usually performed under extra-corporeal circulation (EEC).
- to facilitate the surgical dissection and reduce the bleeding, it is important to avoid too much intravascular volume loading as this increases the venous engorgement of the portal network and the IVC. Volume loading should be guided by the systolic blood pressure, by the variations of its peak value during positive pressure ventilation and also by the observation of the surgical field because some hemodynamic changes are due to transient surgical maneuvers such as mobilization of the liver or compression of a large vessel.
- in case of clamping of the vessels of the hepatic hilum or vascular exclusion of the liver ( = clamping of the vessels of the hilum and the supra- and intra-hepatic IVC), the surgeon must first perform a clamping test to observe the hemodynamic consequences and allow the vascular filling of the child to be adapted before the definitive clamping. Clamping of the hilum is usually well tolerated if the child is not hypovolemic, but vascular exclusion sometimes requires the administration of norepinephrine. If a prolonged clamping is expected, it is best to discontinue it every 15-20 minutes to reduce the ischemic sequelae at the hepatocytic level.
- a risk of gas or tumoral embolism is present throughout the procedure, especially during the dissection and at the time of unclamping of the liver vessels.
- specific case: ex-situ resection of the tumor (rare): the liver is removed entirely from the patient (total hepatectomy) and dissected in an icy conservation fluid to remove the tumor. Given the absence of preoperative portal hypertension, partial extracorporeal venovenous circulation is required to maintain the cardiac output during this anhepatic phase. For example, the introducer of a 8 Fr Swan Ganz catheter can be placed in an internal jugular vein: the lateral arm can be sterilely connected to an heparinized EEC circuit after cannulation of the femoral and portal veins, to ensure a good venous return from the splanchnic field and the lower limbs to the heart.
Jaundice and/or ascites may develop during the first 2 to 5 postoperative days.
Other liver complications are possible:
- bleeding/hematoma on the cut section
- biliary fistula on the cut section: in the absence of externalization by a drain, the first clinical sign is pain (peritoneal irritation by the bile); the diagnosis should also be suspected if the plasma bilirubin level rises because intraperitoneal bile is reabsorbed;
- hepatocytic failure: to be suspected following an extensive hepatectomy and/or total vascular exclusion of the liver. Liver failure is suspected in case of ascites, jaundice, disorders of consciousness (encephalopathy) and clotting defects (INR and low factor V).
References :
- Mazereeuw-Hautier J, Hoeger PH, Benlarech S, Ammmour A, Broue P et al
Efficacy of propranolol in hepatic infantile hemangiomas with diffuse neonatal hemangiomatosis.
J Pediatr 2010 ; 157:340-2.
- Markiewicz-Kijewska M, Kasprzyk W, Broniszczak D, Bacewicz L, Ostoja-Chyzynska A, Ismael H, Kosciesza A et al
Hemodynamic failure as an indication to urgent liver transplantation in infants with giant hepatic hemangiomas or vascular malformations: report of four cases.
Pediatr Transplant 2009; 13:906-12.
- Przybylo HJ, Stevenson GW, Backer C, Luck SR, Webb CL, Morgan E, Hall SC.
Anesthetic management of children with intracardiac extension of abdominal tumors.
Anesth Analg 1994; 78:172-5.
- Lentschener C, Ozier Y.
Anaesthesia for elective liver resection : some points should be revisited.
Eur J Anaesthesiol 2002; 19:780-8.
- Dorman F, Sumner E, Spitz L.
Fatal intraoperative tumor embolism in a child with hepatoblastoma.
Anesthesiology 1985; 63:692-3.
Updated: July 2020