Rare. Part of the bronchopulmonary malformations embryologically derived from the foregut. There is a clear male predominance: 60 to 70% of cases.
The cause is a narrowing of the bronchial lumen due to the absence of or the presence of bronchial cartilage: this causes bronchial collapse at the expiration phase (bronchomalacia), and a one-way valve effect, increasing retention of air in the downstream parenchyma.
The anomaly of cartilage may be due to:
- hypoplasia or agenesis of the bronchial cartilages,
- an anomaly of the composition of the bronchial cartilage (elastin anomaly),
- in utero fibrosis of the interstitium of the bronchial walls,
- extrinsic bronchial compression by a large pulmonary artery during fetal life: the cartilaginous rings, compressed for a long period of time, are malformed.
In 50% of cases, no causative factor is found. In 10% of cases, there are associated malformations, mainly congenital heart disease. A few familial cases with bronchial cartilages hypoplasia and suggesting autosomal dominant transmission have been reported.
Bronchial collapse results in unilateral overstretching of a lung lobe, left upper lobe (41% of cases), right middle lobe (34%) or right upper lobe (21%). As a result, some mediastinal shift and compression of the opposite lung ensue.
The clinical presentation is variable and depends on the importance of the expansion of the pulmonary lobe which can cause a mediastinal shift and block the intrathoracic venous return. The symptoms are similar to those of a tension pneumothorax with severe dyspnea, cyanosis, stridor, respiratory distress, wheezing which is a function of the degree of compression of the normal structures by dystrophic lung parenchyma.
When respiratory distress is severe, urgent surgery is indicated, either by thoracotomy or thoracoscopy. For less severe form, a conservative treatment can be tried either by using controlled ventilation with low pressures and volumes, or by selective intubation of the healthy lung in order to let the diseased lung progressively deflate.
Differential diagnosis : vascular ring, adenomatous lung disease, bronchogenic cyst, bronchomalacia.
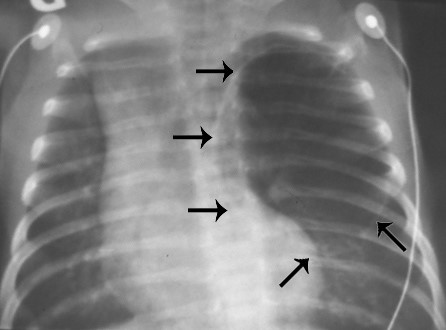
Chest X-Ray shows : localised hyperinflation of the lung with contralateral mediastinal shift and flatening of the ipsilateral diaphragm
Anesthetic implications:
Preoperative echocardiography ; invasive monitoring and unilateral lung ventilation to isolate the diseased lung.
Induction : either by inhalation or intravenous taking care to maintain spontaneous ventilation and to avoid N2O. Spontaneous ventilation should be preserved until the diseased lung is effectively isolated or the thorax is opened in order to avoid hyperinflating the diseased lobe or lung through a ball-valve effect.
One-lung ventilation can be achieved
- either by selective intubation of the healthy side under fibroscopy
- or by isolating the diseased side with a Forgaty catheter or a bronchial blocker adapted to the bronchial diameter.
If hypotension occurs during induction or before clamping the bronchus, it is probably due to the association of decreased thoracic venous return caused by increased pressure in the diseased lung and the hemodynamic effects of the anesthetic agents. This can be corrected by decreasing ventilation pressure and concentration of inhaled anesthetic drugs. Ketamine (1-2 mg/kg IV) is a good choice to obtain anesthesia and hemodynamic stability in this context.
References :
- Ulku R, Onat S, Ozçelik C.
Congenital lobar emphysema: differential diagnosis and therapeutic approach.
Pediatr Int 2008; 50:658-61.
- Ceran S, Altuntas B, Sunam GS, Bulut I.
Congenital lobar emphysema: is surgery routinely necessary?
Afr J Paediatr Surg 2010; 7:36-7.
- Tander B, Yalcin M, Yilmaz B, Ali Karadag C, Bulut M.
Congenital lobar emphysema: a clinicopathologic evaluation of 14 cases.
Eur J Pediatr Surg 2003; 13:108-11.
- Gupta R, Singhal SK, Rattan KN, Chhabra B.
Management of congenital lobar emphysema with endobronchial intubation and controlled ventilation.
Anesth Analg 1998; 86: 71-3.
- Schmidt C, Rellensmann G, Van Aken H, Semik M, Bruessel T, Enk D.
Single-lung ventilation for pulmonary lobe resection in a newborn.
Anesth Analg 2005; 101:362-4.
- Iodice F, Harban F, Walker I.
Anesthetic management of a patient with bilateral congenital lobar emphysema.
Pediatr Anesth 2008; 18: 340-1.
- Subramanyam R Costandi A, Mahmoud M.
Congenital lobar emphysema and tension emphysema.
J Clin Anesth 2016; 29: 17-8.
- Kunisaki SM, Saito JM, Fallat ME, Peter SDS et al.
Current operative management of congenital lobar emphysema in children: a report from the Midwest Pediatric Surgery Consortium.
J Pediatr Surg 2019; 54: 1138-42.
Updated: November 2019