(craniosynostoses)
Prevalence is estimated to be 1 / 2500 live births. Craniostenoses consist in developmental anomalies of the skull consecutive to premature fusion of one or more cranial sutures.
A distinction is made between:
- syndromic craniostenosis (15 %): they involve several sutures and are often associated with other malformations (Crouzon's disease, Apert syndrome, etc.) associated with mutations in the FGFR (Acronym for Fibroblast Growing Factor Receptor) genes in the fibroblast growth factor receptor family (FGFR1, FGFR2, FGFR3, TWIST1, MSX2 and EFNB1).
- non-syndromic craniostenosis (85 %): only one suture is concerned, the cranial volume is preserved but the skull is deformed in the direction perpendicular to the fused suture (see figure).
The main observed cranial deformations are:
- scaphocephaly : anteroposterior lengthening and reduction of the width of the skull by premature fusion of the sagittal suture (between both parietal bones); the most common: 40-50 %; annual incidence: 1/5,000 to 1/8,000 births; sex ratio 3.5/1 and 6 % of family forms
- trigonocephaly : triangular shaped forehead due to the premature fusion of the metopic suture (suture between the right and left parts of the frontal bone); the forehead presents a median edge and its width is reduced; the eyes are close together (hypotelorism), and the face is narrow; annual incidence 1/7,000 to 1/15,000 births; sex ratio 3.3/1, 5.6 % of family forms
- plagiocephaly : antero-lateral flattening of the skull of one side due to early fusion of one of the two coronal sutures (suture between the frontal and the parietal bone); there exists also the so-called deformational plagiocephaly (nonsynostotic), where the deformation does not result from premature fusion of a suture: it is caused by ante- or postnatal head malpositioning. Annual incidence 1/10,000 births; sex ratio 1/2, the right side is more often affected than the left and there are 14 % of familial forms
- brachycephaly : anteroposterior shortening and enlargement of skull secondary to premature fusion of both coronal sutures (and often lambdoid sutures); annual incidence 1/20,000 births; sex ratio 1/2, and 14 % of familial forms; sometimes syndromic
- oxycephaly (or acrocephaly): reduction of width and height of the skull (taking the shape of a tower) as a result of the premature fusion of the metopic, coronal and sagittal sutures.
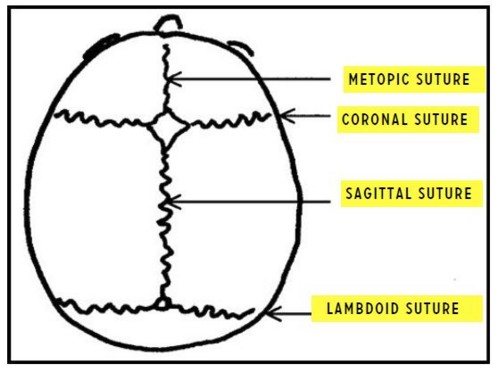
Different types of craniostenoses: doted line -> fused suture
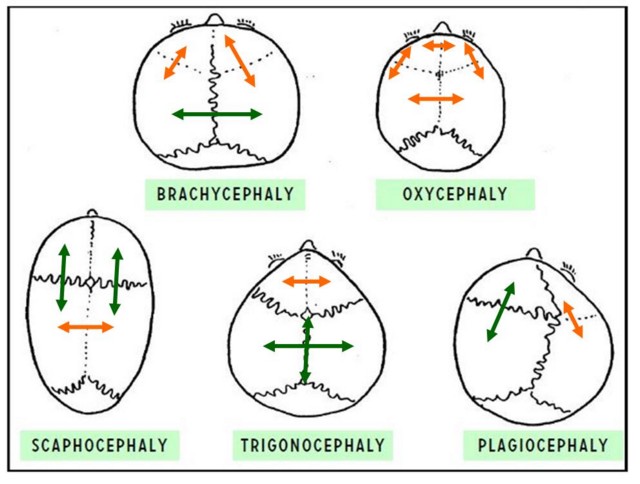
Main forms of craniostenoses: the fused suture is in red
There is no noticeable harm to neurological development when the metopic suture alone is involved. In all other cases, cranial deformity leads to disorders in the development of brain structures and CSF circulation.
Apart from clinically obvious cranial deformity, syndromic craniostenosis can lead to:
- exophthalmos, visual disturbances that can quickly lead to blindness,
- breathing problems (obstructive sleep apnea)
- intracranial hypertension (papillary edema, digitiform impressions at the XRay of the skull or CT scan) and sometimes rapid neurological degradation
- hydrocephaly
- disorders of maxillomandibular occlusion.
The severity of these consequences requires early surgical treatment, ideally between 3 and 6 months. This is a hemorrhagic surgery (loss of a blood mass on average) as soon as more than one suture is involved. The particular risks of this surgery are hemorrhage (which can be massive if a venous sinus is opened), gas embolism (even when lying down) and hypothermia.
Depending on the age of diagnosis and the type of cranial deformity, several types of interventions are feasible:
- linear craniectomy in case of a single suture (< 6 months): the procedure consists of one or more linear craniectomies that remove the prematurely fused suture. This procedure is usually performed as soon as the infant weighs 5 kg.
- endoscopic longitudinal craniectomy (< 6 months): this procedure is less hemorrhagic, is shorter and carries a significantly lower embolic risk than conventional surgery.
- linear craniectomy and placement of springs around 3-6 months to keep the sutures apart; these springs are removed after 8 to 12 weeks. These two interventions are very short and not very hemorrhagic
- remodeling of the cranial vault around 1 year of age, duration 4-6 h.
- fronto-orbital advancement between 12 and 18 months of age, in case of midface hypoplasia
- for syndromic forms: depending on the involved sutures, firstly posterior expansion without or with distraction around 6 months of age; early frontofacial monoblock with distraction from 18 months of age, frontal expansion preceding a facial advancement type Le Fort 3, etc.
Positionings: depending on the surgical approach,
- supine position and slightly raised head,
- ventral decubitus and neck in hyperextension (position of the sphynx),
- rarely sitting.
There is a risk of acute intracranial hypertension at the time of the closure of the skull with bradycardia and hypertension or circulatory collapse. After surgery, the child must wear a modeling helmet for several months to protect the skull and avoid a relapse to its original shape.
Anesthetic implications:
- preoperative:
- simple suture or syndrome ? associated malformations ?
- signs of intracranial hypertension ?
- hemoglobin and coagulation: prescription of iron and/or erythropoietin to increase preoperative Hb levels, blood order
- cardiac ultrasound: malformation ? foramen ovale ?
- evaluation of the upper airways: laryngeal abnormalities ? tracheomalacia ? obstructive sleep apnea ? choanal stenosis ? Chiari malformation ?
- intraoperatively:
- risk of difficult mask ventilation in case of midface hypoplasia, positioning (check in surgical position) and careful fixation of the endotracheal tube;
- placement of 2 peripheral routes and an arterial line (except endoscopic); central venous line
- tranexamic acid: for example, 15 mg/kg followed by 5 mg/kg/h.
- management of hemorrhagic shock or gas embolism: risk of hypotension without reactive tachycardia (trigemino-cardiac reflex ?)
- prevention of hypothermia.
- preoperative temporary tracheostomy in complex cases with LeFort osteotomy?
- postoperative:
bleeding, facial edema, risk of hyponatremia (inappropriate ADH secretion, hypotonic fluids), optimal pain treatment
References :
- Connolly JP, Gruss J, Seto ML, Whelan MF, Ellenbogen R, Weiss A, Buchman SR, Cunningham ML.
Progressive postnatal craniosynostosis and increased intracranial pressure.
Plast Reconstr Surg 2004; 113:1313-23.
- Jimenez DF, Barone CM.
Endoscopic craniectomy for early surgical correction of sagittal craniosynostosis.
J Neurosurg 1998, 88:77-81.
- Meier PM, Goobie SM, DiNardo JA, Proctor MR, Zurakowski D, Soriano SG.
Endoscopic strip craniectomy in early infancy: the initial five years of anesthesia experience.
Anesth Analg 2011; 112: 407-14
- Dadure C, Sauter M, Bringuier S, Bigorre M, Raux O, Rochette A, Canaud N, Capdevila X.
Intraoperative tranexamic acid reduces blood transfusion in children undergoing craniosynostosis surgery.
Anesthesiology 2011; 114: 856-61.
- Erol DD.
A risk during an elective repair of craniosynostosis: the Cushing reflex.
Pediatr Anesth 2007; 17: 496-7
- Meier PM, Guzman R, Erb TO.
Endoscopic pediatric neurosurgery: implications for anesthesia.
Pediatr Anesth 2014 ; 24 : 668-77.
- Teichgraeber JF, Baumgartner JE, Waller AL, Reis SM, Stafford MT, Hollinger LE, Gateno J, Xia JJ.
Microscopic minimally invasive approach to nonsyndromic craniosynostosis.
J Craniofac Surg 2009; 20:1492-500.
- Pearson A,Matava CT.
Anaesthetic management for craniosynostosis repair in children.
BJA Education 2016;1-7
- Bennis Y, Wolber A, Vinchon M, Belkhou A, Duquennoy-Martinot V, Guerreschi P.
Les craniosténoses non syndromiques.
Ann Chir Plast Esth 2016 ; 61:389-407
- Arnaud E, Paternoster G, James S, Morisseau-Durand M-P, Couloigner V, Diner P, Tomat C et al.
Stratégie craniofaciale pour les faciocraniosténoses.
Ann Chir Plast Esth 2016 ; 61:408-19.
- Stricker PA, Lin EE, Fiadjoe JE, Sussman EM, Jobes EM.
Absence of tachycardia during hypotension in children undergoing craniofacial reconstruction surgery.
Anesth Analg 2012 ; 115 : 139-46
- Mattews F, Shaffer AD, Georg MW, Ford MD et al.
Airway anomalies in patients with craniosynostosis.
The Laryngoscope 2019 ; 129 : 2594-602
Updated: May 2022