Prevalence: about 1/200,000 live births. It seems to be more frequent in girls (ratio 3:1). By definition: twins (sometimes with different ADN) joined by a part of their body. This anomaly is an accident of embryonic development (default of fission or secondary fusion). It only occurs in monoamniotic monochorionic twin pregnancy.
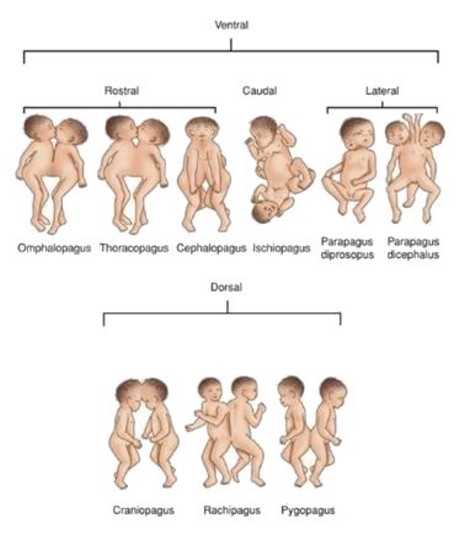
Classification: (pagos = fixed in Greek παγοσ)
- ventral junction (front line) [87 %]
1 cephalopagus (11 %): fusion from the top of the skull to the umbilicus; often death in utero
2 thoracopagus (19 %): fusion at the level of the chest; the most frequent form; shared liver (100 %), joint pericardium (90 %) and heart (75 %)
In case of cardiac fusion = cardiopagus type:
- A: hearts are completely separate
- B: hearts are separated within a common pericardium
- C: the atria are joined but the ventricles are separated
- D: the atria and the ventricles are common.
3 omphalopagus (18 %): fusion of the lower part of the chest up to the navel.
4 xiphopagus : joined by the xiphoid appendix; common liver (81 %), digestive (31 %) or heart (25 %) malformations
- caudal junction: ischiopagus (1 %): fusion at the pelvis level, either face-to-face or head to tail; joint parts at the urogenital and lombosacral levels, variable number of limbs malformations
- lateral junction (28 %): parapagus: lateral fusion from the pelvis with different junctions at the level of the chest (dipagus or dithoracic), of the head with two faces (diprosopus) or of the skull (dicephalus)
- dorsal junction (neural tube) [13 %]
1 craniopagus (5 %): fusion at the level of the vault of the skull without including the face:
- type A: only the scalp and the subcutaneous tissue are joined
- type B: the dura is common
- type C: the dura and the arachnoid are common
- type D: brain tissue is shared
2 rachipagus (2 %): fusion of the spinal column on the middle line
3 pygopagus (6 %): fusion at the level of the sacrum, the coccyx and the perineum (18-28 %). often sharing of the rectum or the anus, the bladder and nerve structures.
The classification can be extended according to the number of involved limbs :
- dibrachius: 2 upper limbs
- tribrachius: 3 upper limbs
- tetrabrachius: 4 upper limbs
- dipus: 2 lower limbs
- tripus: 3 lower limbs
- tetrapus: 4 lower limbs.
Modified from: Spencer R.
Conjoined twins: developmental malformations ad clinical implications. Baltimore, John Hopkins Univ. Press, 2003.
A minimal form of Siamese twins is called heteropagus (see this term) or parasitic twin where the major part of one of the twins has involuted and the remnant takes the form of an external or internal outgrowth.
Treatments:
- abstention: either palliative care until death or children are allowed to grow up as they are
- surgical separation in emergency: in case of injury of the shared tissue or when one of the twins jeopardizes the survival of the other or when the medical condition of the twins deteriorates (cardiac or respiratory factors) or when the medical condition of one of the twins is incompatible with survival while the other is viable.
- programmed splitsing
Anesthetic implications:
- define as precisely as possible (X-Rays) the type of fusion, especially which organs and structures are shared; echocardiography, 3D reconstruction. In case of cross-circulation (at the cardiac or hepatic level) between the twins, a poor balance caused by differing flows (following a cardiac malformation, for example), can result in an ex-utero equivalent of the TTTS (Twin-to-Twin Transfusion Syndrome) (one hypervolemic twin and the other hypovolemic) whose management requires a rapid separation
- several anesthesias are often necessary either to perform preoperative examinations (MRI, angiography etc.) or to perform palliative procedures (colostomy): the management of the airways and of a possible cross-circulation is the same as for the separation surgery
- in absence of isotopic tests or angiography to determine the presence or absence of a cross-circulation, an atropine test can be performed: inject a dose of atropine in a twin and watch if the second becomes tachycardic within 5 minutes.
- clearly discuss in advance with the parents how the organs/limbs will be allocated and which twin takes precedence in case of major difficulties
- basic principles: clearly identify both children as well as their I.V. lines, ventilation tubes and monitoring with a color code. At least one anesthesiologist is assigned to each twin
- separation surgery: must be simulated during a session with two dolls. All phases of the intervention must be simulated: intubation, surgical positioning, separation and transport to a second surgical table. There will be two specifically allocated ventilators even if some teams have used a synchronous ventilation of both twins by connecting their tracheal tubes with the special connecting device used for one lung ventilation in adults (Carlen’s conector).
- in case the twins are joined face to face or are connected at the level of the upper chest (thoracopagus, omphalopagus, craniopagus), or in case of hyperextension of the head (omphalopagus), control of the airways and tracheal intubation can be difficult, even in the absence of micro-retrognathism: it is necessary either to intubate each child turned on his side either to turn one child on his back while the other is held overhead by an helper (and reversing the positions for intubation of the second twin); in case of cross-circulation, positioning one of the twins above the other puts him at risk of collapse and the other at risk of autotransfusion. Intubate preferably with armed tubes.
- hydro-electrolytic requirements: calculation taking the total weight of the twins into account and administer 50% of the volume to each one
- prevention of hypothermia
- risk of massive hemorrhage and coagulopathy by hemodilution
- risk of major hypotension during separation: it is generally due to hypovolemia
- post-operative period: risk of bleeding, of failure of a split organ, of skin defects (even if skin expanders have been placed in preoperative), of abdominal or thoracic compression if the sutures are too tight
- in case of ischiopagus or pygopagus: check the absence of spinal cord abnormalities (duplication, attached spinal cord) before performing a neuraxial block
- post-operative period: put the twins close to one another as soon as possible
E.jpg)
omphalopagus twins operated in emergency (ruptured omphalocele) at birth (UCL St Luc, Brussels)
References :
- Walton JM, Giacomantonio JM, Hayashi AH.
Emergency separation of conjoined twins.
J Pediatr Surg 1991 ; 26 : 1337-40
- Spencer R.
Anatomic description of conjoined twins: a plea for standardized terminology.
J Pediatr Surg 1996 ; 7 : 941-4
- Seefelder C, Hill DR, Shamberger RC, Holzman RS.
Awake caudal anesthesia for inguinal surgery in one conjoined twin.
Anesth Analg 2003; 96 : 412-3
- Thomas JM , Lopez JT.
Conjoined twins: the anaesthetic management of 15 sets from 1991-2002.
Pediatr Anesth 2004; 14: 117-29
- Pietrini D, Valenti M, Pusateri A, Scorzoni M, Tosi F, Forte E, Barbi S, Caresta E et al.
Perioperative management of face-to-face craniopagus twins separation
Pediatr Anesth 2005; 15: 519-24
- Szmuk P, Rabb MF, Curry B, Smith KJ, Lantin-Hermoso MR, Ezri T.
Anaesthetic management of thoracopagus twins with complex cyanotic heart disease for cardiac assessment: special considerations related to ventilation and cross-circulation.
Br J Anaesth 2006; 96: 341-5.
- Parameswari A, Vakamudi M, Raghupathy V, Siddadharta R.
Anaesthetic management of total craniopagus twins for magnetic resonance imaging and cerebral angiography.
Br J Anaesth 2010; 105: 368-70
- Singh M, Jacob R, Naik V, Baines D.
Separation of thoraco-omphalopagus twins in a rural secondary hospital: perioperative management.
Ind J Anaesth 2012; 56:
- Yousuf MS, Shamim F, Dogar SA, Khan FA.
Anesthetic management of conjoined twins for computed tomography scan.
A&A Case Reports 2016; 7: 181-3
- Thomas J.
Anesthesia for conjoined twins
in Smith’s Anesthesia for infants and Children, 8th ed by Davis PJ, Cladis FP, Motoyama E. Elsevier 2011, p 950-70
- Frawley G.
Conjoined twins in 2020: state of the art and future directions.
Curr Opin Anaesthesiol 2020; 33:381-7
- Kiss E, Chehab S, Moreno Duarte I, Khan U, Schindel D, Pandya S, Ullah S, Ochoa C, Zabala LM.
Twin-twin transfusion syndrome complicated by single ventricle physiology: a case report.
Pediatr Anesth 2021; 31:1255-8
Updated: October 2021