(acronym for Calcium-Release Deficiency Syndrome, VACRDS, acronym for Ventricular Arrhythmias due to Cardiac Ryanodine Receptor calcium release Deficiency Syndrome)
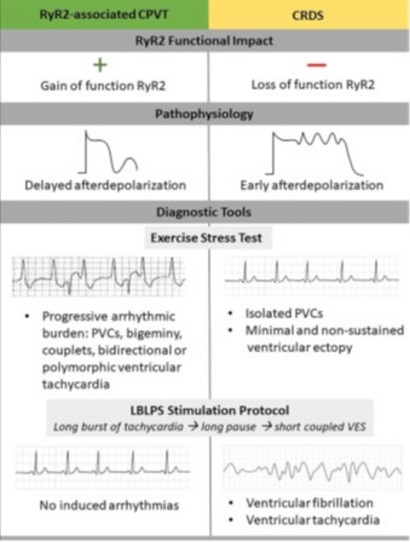
Very rare. Autosomal dominant transmission of a loss-of-function mutation of the RYR2 gene (1q43), resulting in early afterdepolarization of the cardiomyocytes. Gain-of-function mutations of the same gene can cause catecholaminergic polymorphic ventricular tachycardia type 1 [MIM 604 772] and arrhythmogenic right ventricular dysplasia type 2 [MIM 600 996] (see these terms). Ventricular rhythm disorder characterized by syncope, cardiac arrest or sudden death, often referred to as idiopathic ventricular fibrillation. Polymorphic ventricular tachycardia and ventricular fibrillation have also been described. These symptoms are usually triggered by exercise or emotional stress, but cannot be induced by exercise testing or adrenaline testing, unlike typical catecholaminergic polymorphic ventricular tachycardia.
An electrophysiological test in which the appearance of the first beat after the pause following a tachycardia (> 120 or 150 bpm, induced by pacing or spontaneous) is analyzed would enable the diagnosis to be made: the amplitude of the T wave and its width are greater than before tachycardia and than in patients suffering from another arrhythmogenic pathology.
In some cases, non-compaction of the left ventricle, dilated cardiomyopathy or QT prolongation can be observed.
Treatment: given the rarity of the syndrome, treatment is poorly established: beta-blockers are controversial, flecainamide, automatic internal defibrillator, etc.
Anesthetic implications:
this diagnosis should be kept in mind in case of familial history of sudden death or ventricular tachycardia during exertion. Major risk of sudden death in the perioperative period. There is no risk of malignant hyperthermia despite the mutation of the cardiac isoform of the ryanodine receptor gene; ready-to-use esmolol or flecainamide and defibrillation pallets in place; avoid stress (premedication, presence of a parent). By analogy with catecholaminergic polymorphic ventricular tachycardia, avoid ketamine because it induces tachycardia.
In case of cardiac arrest: low doses of adrenaline as it could worsen rhythm disorders and amiodarone is ineffective.
In case of locoregional block: avoiding the addition of adrenaline to the local anesthetic solution ?
Avoid all triggering factors of cardiac rhythm disorders: hypoxia, hypercarbia, hypovolemia, light anesthesia, placement of a Swan-Ganz catheter.
References :
- Sawn H, Laitinen PJ, Toivonen L.
Volatile anesthetics and succinylcholine in cardiac ryanodine receptor defects.
Anesth Analg 2004 ; 99 : 435
- Staikou C, Chondrogiannis K, Mani A.
Perioperative management of hereditary arrhythmogenic syndromes.
Br J Anaesth 2012; 108: 730-44.
- Sun B, Yao X, Ni M, Guo JWZ, Wang LZ et al.
Cardiac ryanodine receptor calcium release deficiency syndrome.
Science Translational Medicine 2021 ; 13, Issue 579, DOI: 10.1126/scitranslmed.aba7287
- Roston TM, Wei J, Guo W, Li Y, MD, Zhong X, Wang R, Estillore JP, Peltenburg PJ et al.
Clinical and functional characterization of Ryanodine receptor 2 variants implicated in Calcium-Release Deficiency Syndrome.
JAMA Cardiol. doi:10.1001/jamacardio.2021.4458
- Kallas D, Roberts JD, Sanatani S, Roston TM.
Calcium Release Deficiency Syndrome : a new inherited arrhythmia syndrome.
Card Electrophysiol Clin 2023 ; 15 : 319-29
- Ni M, Dadon Z, Ormerod JOM, Saenen J, Hoeksema WF, Antiperovitch P, Tadros R, Christiansen MK et al.
A clinical diagnostic test for Calcium Release Deficiency Syndrome.
JAMA. doi:10.1001/jama.2024.8599
Updated: June 2024