Prevalence 1/2,000 to 5,000 in Europa. Cause of syncope and sudden death at rest by ventricular fibrillation in young adults. Strong male predominance (10:1) after puberty; it seems that estrogen could have an antiarrhythmic role in women. This syndrome is common among young men in Japan and Southeast Asia. It may present as atrial fibrillation in children.
It is a channelopathy of of the Na (types 1, 2, 5 and 7), K (type 6, 9) or Ca (types 3 and 4) cardiac epicardial channels, especially at the level of the ejection pathway of the right ventricle.
The transmission is autosomal dominant.
From a genetic point of view, a distinction is made between:
- type 1 [MIM 601 144] (20 -30 %): mutation of the SCN5A gene (3p21); it can also produce the LQT3 type long QT syndrome
- type 2 [MIM 611 777]: mutation of the GPD1L gene (3p22)
- type 3 [MIM 611 875]: mutation of the CACNA1C gene (12p13) and type 4 [MIM 611 876]: mutation of the CACNB2 gene (10p12). They may also present as a short QT syndrome
- type 5 [MIM 612 838]: mutation of the SCN1B gene (19q13)
- type 6 [MIM 613 119]: mutation of the KCNE3 gene (11q13)
- type 7 [MIM 613 120]: mutation of the SCNB3 gene (11q24)
- type 8 [MIM 613 123]: mutation of the HCN4 gene (15q24)
- type 9 [MIM 616 399]: mutation of the KCND3 gene (1p13)
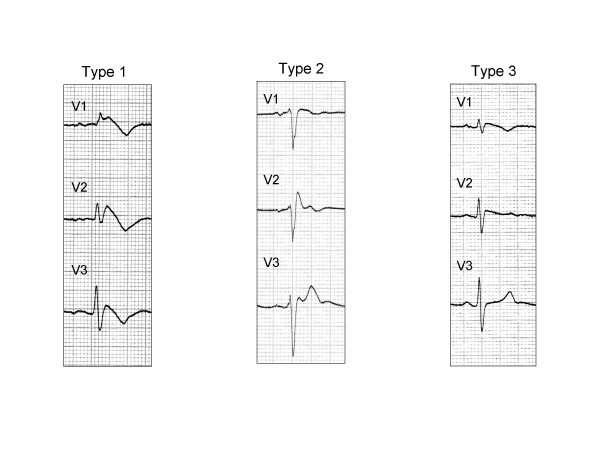
Three types of ECG tracings (non-ischemic modifications in V1 - V3) are described: the 3 types present a wide QRS similar to a right bundle branch block followed with:
Type 1 (kown as typical): a dome-shaped elevation ('coved') of the segment ST >= 2 mm (especially in V1) the ascending part of which is short: it is followed by a symmetrical reverse T-wave in V1 and V2
Type 2 (known as atypical ): "saddle" shaped ST-segment elevation of point J >= 2 mm and elevation of the ST > 1 mm, followed by a positive or biphasic T wave
Type 3 (known as atypical): looks like type 2, but is more flattened with an elevation of J point <= 1 mm
Some cardiologists believe that Brugada syndrome and idiopathic ventricular fibrillation with a high J wave and elevation of the ST-segment are part of spectrum of phenotypic expression called the 'J-wave syndromes'
These recordings are sometimes intermittent and unmasqued by fever, vagal stimulation, or sleep, and disappear during an effort or following the administration of isoprenaline. All types can be present in a successive way in the same patient. Because the type 2 and 3 ECG patterns are less specific, pharmacological tests have to be performed to confirm the diagnosis: either with ajmaline (1 mg/kg in 5 minutes) or flecainide (2 mg/kg in 10 minutes).
The term of Brugada syndrome is used when an ECG type 1 tracing is associated with an episode of polymorphic ventricular tachycardia or ventricular fibrillation, with a family history of SIDS under the age of 45 years or with unexplained syncope .
Treatment with hydroquinidine seems effective. An implantable defibrillator is inserted in case of episodes of arrhythmias associated with an abnormal ECG at rest; it can sometimes be associated with a pacemaker in case of sick sinus syndrome.
Useful reference : www.brugadadrugs.org
Sometimes ones refers to a " acquired Brugada syndrome " when a typical ECG pattern appears under the influence of a pharmacological treatment (mostly continuous infusion of propofol where this change may announce a propofol infusion syndrome), with or without fever, in a patient whose ECG was previously normal.
Anesthetic implications:
If an internal defibrillator is implanted, turn it off before the surgical procedure because the electrocautery may trigger defibrillation; defibrillation patches should be placed on the chest to defibrillate whenever necessary during the procedure. Monitoring is adapted to the importance of surgery: it is prudent to use a 5-lead ECG and do not hesitate to insert an arterial catheter.
In case of intraoperative ST segment elevation, it is useful to start an infusion of isoproterenol.
Avoid:
- any vagal stimulation and beta -blockers;
- sympathetic stimulation: perioperative analgesia is necessary
- neostigmine which increases the elevation of ST segment in this context;
- hyperthermia;
Sevoflurane is the halogenated agent of choice. All intravenous anesthetics have been used without problem, including propofol in a single dose or as continuous infusion. However several reported cases of PRIS (Propofol Infusion Syndrome) presented with an ECG similar to a Brugada syndrome shortly before the occurrence of rhythm disorders and, conversely a few cases of arrhythmias following the administration of propofol have been reported in patients with Brugada syndrome.
Decreased doses of local anesthetics (which block Na+ channels ) especially bupivacaine (except for spinal anesthesia). In a series of 47 locoregional anesthesias, only 1 case of ventricular fibrillation was reported, following the diagnostic injection of ajmaline 60 min after chest block.
References :
- Mivelaz Y, Di Bernardo S, Pruvot E, Meijboom EJ, Sekarski N.
Brugada syndrome in childhood : a potential fatal arrhythmia not always recognized by paediatricians. A case report and review of the literature.
Eur J Pediatr 2006; 165: 507-11.
- Phillips N, Priestley M, Denniss AR, Uther JB.
Brugada-type electrocardiographic pattern induced by epidural bupivacaine.
Anesth Analg 2003; 97: 264-7
- Vernooy V, Sicouri S, Dumaine R, Hong K, Oliva A, Burashnikov E, Timmermans C, Delhaas T, Crijns HJGM, Antzelevitch C, Rodriguez L-M, Brugada R.
Genetic and biophysical basis for bupivacaine-induced ST segment elevation and VT/VF. Anesthesia unmasked Brugada syndrome.
Heart Rhythm 2006; 3 : 1074-8.
- Probst V, Denjoy I, Amirault J-C et al.
Clinical aspects and prognosis of Brugada syndrome in children.
Circulation 2007; 115: 2042-8.
- Canbay O, Erden IA, Celebi N, Aycan IO, Karagoz AH, Aypar U.
Anesthetic management of a patient with Brugada syndrome.
Pediatr Anesth 2007, 17: 1225-6.
- Baty L, Hollister J, Tobias JD.
Perioperative management of a 7-year-old child with Brugada syndrome.
J Intens Care Med 2008; 23: 210-4.
- Robinson JDC, Melman Y, Walsh EP.
Cardiac conduction disturbances and ventricular tachycardia after prolonged propofol infusion in an infant.
PACE 2008; 31: 1070-3
- Cordery R, Lambiase P, Lowe M, Ashkey E.
Brugada syndrome and anesthetic management.
J Cardiothor Vasc Anesth 2006; 20: 407-13.
- Carey SM, Hocking G.
Brugada syndrome – a review of the implications for the anaesthetist.
Anaesth Intensive Care 2011; 39: 571-7.
- Bramall J, Combeer A, Springett J, Wendler R.
Caesarian section for twin pregnancy in a parturient with Brugada syndrome.
Int J Obstetr Anesth 2011; 20: 181-4.
- Staikou C, Chondrogiannis K, Mani A.
Perioperative management of hereditary arrhythmogenic syndromes.
Br J Anaesth 2012; 108: 730-44.
- Meggiolaro M, Zorzi A, El Maghawry M, Peruzza F, Migliore F, Pittoni GM.
Brugada ECG disclosed by acute malaria: is it all about fever and propofol?
J Clin Anesth 2013; 25: 483-7.
- Lin Y-C, Chen C-C, Yang C-C.
Perioperative isoproterenol infusion in a patient with Brugada syndrome.
Can J Anesth 2017; 64: 552-3.
- Aytuluk HG.
Cardiac arrest during spinal anaesthesia in a patient with undiagnosed Brugada syndrome.
Eur J Anaesthesiol 2018; 35: 711-3
- Flamée P, Varnavas V, Dewals W, Carvalho H et al.
Electrocardiographic effects of propofol versus etomidate in patients with Brugada syndrome.
Anesthesiology 2020; 132: 440-51.
- Ranucci M.
Challenge of anesthesia management in Brugada syndrome.
Anesthesiology 2020, 132: 411-2.
- Flamée P, Viaene K, Tosi M, Carvalho HN, de Asmundis C, Forget P, Poelaert J.
Propofol for induction and maintenance of anesthesia in patients with Brugada syndrome: a single-center, 25-year, retrospective cohort analysis.
Anesth Analg 2021; 132:1645-53.
- DeLeon AM, Gaiha RD, Peralta FM.
The successful anesthetic management of a cesarean delivery in a patient with Fanconi–Bickel syndrome.
Case Reports in Anesthesiology 2022: 3220486, doi 10.1155/2022/3220486
- Tosi M, Flamée P, Scholliers A, Opsomer T, Raeymaeckers S, Vanhonacker D.
Locoregional anesthesia in patients with Brugada syndrome. A retrospective database analysis.
Acta Anaesth Scand 2025; 69: e14564; doi.org/10.1111/aas.14564
- Luedi MM, Rickli H, Sauter AR.
Exploring locoregional anaesthesia in Brugada syndrome: balancing risk with innovation.
Acta Anaesth Scand 2025; 69: doi 10.1111/aas.14586
Updated: March 2025