New denomination for Congenital airway malformation
Estimated prevalence of 1/25,000 to 30,000 births but it seems to be more frequent since prenatal screening has been established.. Congenital cystic lung malformation caused by an anomaly of lung development disturbing its downstream bronchial, bronchiolar or alveolar expansion. The more proximal the lesion, the more severe it is and the earlier it becomes symptomatic (figure). The lesion develops in utero, is generally detected during the second trimester of the gestation (± echogenic mass in the lung) and reaches its maximum size on the 25th week of intrauterine life. This is one of the possible causes of fetal hydrops or polyhydramnios. It tends to regress later and may even disappear before birth. It is more common on the left side and is bilateral in 5-15 % of cases.
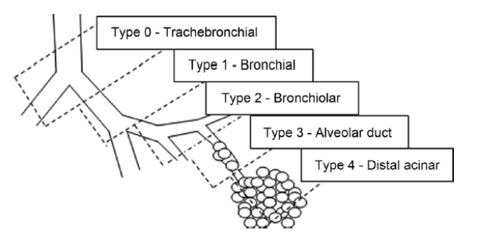
According to the site of initial anomaly, 5 types of congenital airway malformations are recognized (Stocker's classification):
- type 0 : rare, fatal: acinar dysplasia with no alveolar development beyond the pseudoglandular stage
- type 1: the most frequent (50-70 %), characterized by the presence of one or several large cysts ;
- type 2: (15-30 %) with one large mass, cystic or not
- type 3: (5-10 %) with multiple small cysts
- type 4: (5-10 %) purely alveolar defect where large cysts replace the alveolar cavities at the periphery of the lobe. Radiologic picture similar to type I pleuropulmonary blastoma.
Types 1, 2 and 4 are generally of the macrocystic type while type 3 is microcystic. Some cases, known as hybrid, combine a malformation of the airways and a pulmonary sequestrum (see pulmonary sequestration).
In case of polyhydramnios, hydrops foetalis or compression of the heart by the mass, corticotherapy, percutaneous sclerotherapy of the lesions (type 2 or 3) or insertion of a thoraco-amniotic shunt (type 1 or 4) can be tried. A procedure of the EXIT type is sometimes necessary at birth.
Newborns in severe respiratory distress (hyperinflation of the affected lung, mediastinal shift, compression of the healthy lung, sometimes pulmonary hypertension) require emergency surgery.
Asymptomatic newborns (70 %) are either monitored regularly (some lesions gradually disappear) or scheduled for elective surgery preferably before 6 months of age. It happens that the malformation is not recognized in utero and then remains asymptomatic for a long time: its diagnosis is then often fortuitous (repeated infections, pneumothorax). The risk of subsequent pleuropulmonary blastoma (see this term) in non-operated children appears to be low unless there is a mutation of the DICER gene.
The affected lobe is increased in size and presents with disorganization of the bronchial structures. The thoracic CT or MRI reveals the presence of multiple cysts within the lesion, which is not usual in congenital Lobar emphysema (see this term).
Surgical treatment consists of a simple lobectomy, that usually does not require any lung exclusion during surgery (see below).


Anesthetic implications:
check hemoglobin saturation at room air; XRay of the chest: hyperinflation on the affected side ? mediastinal shift ? Echocardiography: pulmonary hypertension ? In case of pulmonary hyperinflation, avoid positive pressure ventilation until the involved lung is excluded (selective intubation of the opposite side or blockade of the affected side) or the chest is open; in the microcystic forms, the malformation often contains fluid and there is a risk of contamination of the airway (induction period, surgical manipulations). According to these elements, contact with the surgeon to decide whether single lung ventilation, is useful. Risk of hemorrhage.Thoracic epidural or paravertebral block for postoperative analgesia.
References :
- Politis GD, Baumann R, Hubbard AM.
Spillage of cystic pulmonary masses into the airway during anesthesia.
Anesthesiology 1997; 87:693-6.
- Mendeloff EN.
Sequestrations, congenital cystic adenomatoid malformations, and congenital lobar emphysema.
Semin Thorac Cardiovasc Surg 2004; 16:209-14.
- Laberge JM, Puligandla P, Flageole H.
Asymptomatic congenital lung malformations.
Semin Pediatr Surg 2005; 14:16-33.
- Lakhoo K.
Management of congenital cystic adenomatous malformations of the lung.
Arch Dis Child Fetal Neonatal Ed 2009; 94:F73-6.
- Guruswamy V, Roberts S, Arnold P, Potter F.
Anaesthetic management of a neonate with congenital cyst adenoid malformation.
Br J Anaesth 2005; 95: 240-2.
- Subramanyam R, Ledbetter K, Fleck R, Mahmoud M.
Images in Anesthesiology: congenital pulmonary airway malformation.
Anesthesiology 2017; 127: 382
- Leblanc C, Baron M, Desselas E, Hanh Phan M, Rybak A, Thouvenin G, Lauby C, Irtan S.
Congenital pulmonary airway malformations: state-of-the-art review for pediatrician’s use.
Eur J Pediatr 2017 ; 176:1559-71
- Johansen M., Veyckemans F., Engelhardt T.
Congenital anomalies of the large intrathoracic airways.
Pediatr Anesth 2022; 32: 126-37
- Karlsson M, Conner P, Ehren H, Bitkover C, Mesas Burgos C.
The natural history of prenatally diagnosed congenital pulmonary airway malformations and bronchopulmonary sequestrations.
J Pediatr Surg 2022 ; 57 : 282-7
Mise-à-jour November 2022